Its tick season, Are you ready?
Its that time of year again. Along with lovely, warm, sunny days, gardens in full production, Long walks along winding paths through the woods comes the emergence of the dreaded tick. Honestly, I haven’t found ticks to be of much good use other than food for birds, frigs, spiders and other animals. They carry many disease and can be difficult to find on the body.
Although ticks are commonly thought of as insects, they are arachnids like scorpions, spiders and mites. Ticks are among the most efficient carriers of disease because they attach firmly when sucking blood, feed slowly and may go unnoticed for a considerable time while feeding.
There are two types of ticks that infect humans. The first is the Ixodidae, known as the hard tick. This tick is the most common tick that bites and infects humans. The other is the Argasidae, known as the soft tick.
Where are ticks found

Ticks are usually found outdoors in wooded and grassy areas but are also found in cabins, woodpiles, and caves. They can even be found on your dog after a romp through the grass!
They way ticks find their next meal/host is by detecting the animal’s breath and body odors, by sensing bod heat, moisture, and vibrations. They wait for a host by resting on the tips of grasses and shrubs along well traveled paths. Since they can’t fly or jump, they rest on the tips of grasses or shrubs in a position known as “questing/ From there the ticks latch on to its host.
How ticks spread disease
Some ticks will attach quickly, and others will wander, looking for places like the ear, or other areas where the skin is thinner.
- Depending on the tick species and its stage of life, preparing to feed can take from 10 minutes to 2 hours. When the tick finds a feeding spot, it grasps the skin and cuts into the surface.
- The tick then inserts its feeding tube. Many species also secrete a cement-like substance that keeps them attached during the meal. The feeding tube can have barbs which help keep the tick in place.
- Ticks also can secrete small amounts of saliva with anesthetic properties so that the animal or person can’t feel that the tick has attached itself. If the tick is in a sheltered spot, it can go unnoticed.
- A tick will suck the blood slowly for several days. If the host animal has a bloodborne infection, the tick will ingest the pathogens with the blood.
Many ticks go through life cycles that can span 3 years and go between different hosts. In this way they can widely spread disease between hosts.
Common tickborne diseases
Ticks can be infected with bacteria, viruses or parasites. Some of the most common tick-borne diseases in the United States include: Lyme disease, babesiosis, ehrlichiosis, Rocky Mountain Spotted Fever, anaplasmosis, Southern Tick-Associated Rash Illness, Tick-Borne Relapsing Fever, and tularemia. Other tick-borne diseases in the United States include: Colorado tick fever, Powassan encephalitis, and Q fever.
Lyme disease is probably the most well known tickborne disease, however there are several other diseases that ticks carry. For instance, the Lone Star tick can carry Heartland virus which can cause severe illness and even death. The Lone Star tick also can cause an allergic reaction called alpha gal syndrome which causes the host to become allergic to red meat.
A new CDC study discovered the blacklegged tick, which is found in the eastern half of the US can spread seven diseases. They are listed below:
| Pathogen |
Disease |
States |
Counties |
| Borrelia burgdorferi |
Lyme disease |
30* |
476 |
| Borrelia miyamotoi |
Hard tick relapsing fever |
25* |
271 |
| Anaplasma phagocytophilum |
Anaplasmosis |
24* |
291 |
| Babesia microti |
Babesiosis |
17 |
154 |
| Powassan virus |
Powassan virus disease |
6 |
55 |
| Borrelia mayonii |
Lyme disease |
4 |
12 |
| Ehrlichia muris eauclairensis |
Ehrlichiosis |
2 |
11 |
Lyme Disease
The most widely known and reported tickborne disease that is most likey very underreported is Lyme disease:- approximately 30,000 cases are reported every year, however insurance statistics put the yearly total at more than 476,000 cases that are diagnosed and treated every year.
Lyme disease can be treated effectively with a single dose of doxycycline if diagnosed soon after bitten. (Note that the Jase case is equipped with doxycycline as one of the five antibiotics) If treatment is delayed, Lyme disease can manifest in many debilitating diseases, such as arthritis, facial paralysis, rashes, fevers.
Initial rash of Lyme disease (Erythema Migrans rash) is caused by the bacterium Borrelia burgdorferi and rarely, Borrelia mayonii.
Below is an image of early stages of the rash. More information can be found on the CDC website under Lyme disease.

Prevention of Tick-Borne diseases
There are so many different diseases that are caried by ticks, that many health practitioners aren’t aware of all the diseases and symptoms. It would be almost impossible for your health practitioner to know each tick exposure and associated diseases. It is the responsibility of the individual to know the common ticks and diseases they may carry when venturing outdoors. The CDC has an extensive website on disease causing ticks.
Prevention- avoid exposure: taken directly from the CDC website:
Tick exposure can occur year-round, but ticks are most active during warmer months (April-September). Know which ticks are most common in your area.
Before You Go Outdoors
Know where to expect ticks. Ticks live in grassy, brushy, or wooded areas, or even on animals. Spending time outside walking your dog, camping, gardening, or hunting could bring you in close contact with ticks. Many people get ticks in their own yard or neighborhood.
Treat clothing and gear with products containing 0.5% permethrin. Permethrin can be used to treat boots, clothing and camping gear and remain protective through several washings. Alternatively, you can buy permethrin-treated clothing and gear.
Use Environmental Protection Agency (EPA)-registered insect repellents containing DEET, picaridin, IR3535, Oil of Lemon Eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. EPA’s helpful search tool can help you find the product that best suits your needs. Always follow product instructions. Do not use products containing OLE or PMD on children under 3 years old.
Avoid Contact with Ticks
Avoid hiking through wooded and brushy areas with high grass and leaf litter. Walk in the center of trails. Keep lawns mowed, weeds to a minimum in the yard.
After You Come Indoors
Check your clothing for ticks. Ticks may be carried into the house on clothing. Any ticks that are found should be removed. Tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors. If the clothes are damp, additional time may be needed. If the clothes require washing first, hot water is recommended. Cold and medium temperature water will not kill ticks.
Examine gear and pets. Ticks can ride into the home on clothing and pets, then attach to a person later, so carefully examine pets, coats, and daypacks. Consider tick preventative medication or collars for your pets.
Shower soon after being outdoors. Showering within two hours of coming indoors has been shown to reduce your risk of getting Lyme disease and may be effective in reducing the risk of other tickborne diseases. Showering may help wash off unattached ticks and it is a good opportunity to do a tick check.
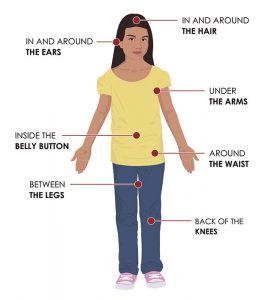
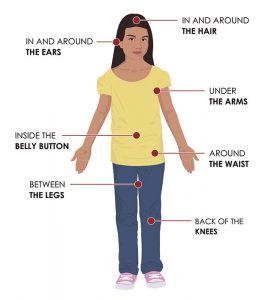
Check your body for ticks after being outdoors. Conduct a full body check upon return from potentially tick-infested areas, including your own backyard. Use a hand-held or full-length mirror to view all parts of your body. Check these parts of your body and your child’s body for ticks:
- Under the arms
- In and around the ears
- Inside belly button
- Back of the knees
- In and around the hair
- Between the legs
- Around the waist
Create a tick safe zone to reduce or eliminate ticks in your backyard.
From the CDC website:
The Connecticut Agricultural Experiment Station has developed a comprehensive Tick Management Handbook for preventing tick bites. Here are some simple landscaping techniques that can help reduce blacklegged tick populations:
- Remove leaf litter.
- Clear tall grasses and brush around homes and at the edge of lawns.
- Place a 3-ft wide barrier of wood chips or gravel between lawns and wooded areas to restrict tick migration into recreational areas.
- Mow the lawn frequently.
- Stack wood neatly and in a dry area (discourages rodents).
- Keep playground equipment, decks, and patios away from yard edges and trees.
- Discourage unwelcome animals (such as deer, raccoons, and stray dogs) from entering your yard by constructing fences.
- Remove old furniture, mattresses, or trash from the yard that may give ticks a place to hide.
Essential oils as tick repellant
A word about essential oils and their efficacy in acting as a tick repellent:
There are many claims about essential oils used as an effective tick repellant on the internet. Some point to studies done on selected ticks and make claims that these oils are just as effective as DEET. Cedarwood, cinnamon, lemon eucalyptus, oregano oil(this oil was the most effective) and other oils have demonstrated a level of repellant qualities, however they must be applied ever few hours and are not as effective as DEET. . Most of these claims are somewhat correct, however they are not as effective as DEET.
The product BioUD with the active ingredient 2-undecanone found in the wild tomato was found is as effective as DEET in repelling ticks. This product is no longer available.
How to remove a tick
The following is directly from the CDC website on tick removal, they have a “tick bot” that can guide you through the process of safely removing the tick if you should happen to find one embedded in your skin.

Use clean, fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible.
Pull upward with steady, even pressure. Don’t twist or jerk the tick; this can cause the mouthparts to break off and remain in the skin. If this happens, remove the mouthparts with tweezers. If you cannot remove the mouth easily with tweezers, leave it alone and let the skin heal.
After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.
Never crush a tick with your fingers. Dispose of a live tick by
- Putting it in alcohol,
- Placing it in a sealed bag/container,
- Wrapping it tightly in tape, or
- Flushing it down the toilet.
Follow-up
If you develop a rash or fever within several weeks of removing a tick, see your doctor:
- Tell the doctor about your recent tick bite,
- When the bite occurred, and
- Where you most likely acquired the tick.
- Avoid folklore remedies such as “painting” the tick with nail polish or petroleum jelly, or using heat to make the tick detach from the skin. Your goal is to remove the tick as quickly as possible–not waiting for it to detach.
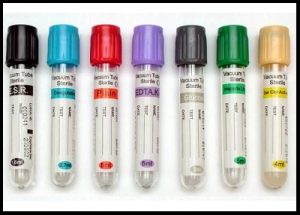
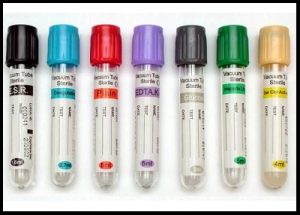
January 18,2022 the FDA issued a supply shortage of every type of blood collection tubes. These tubes are used in blood coagulation tests, drug and hormone levels, to basic chemistry and hematology tests, and provide the foundation the health practitioner needs to diagnose and treat patients.
The primary US based tube manufacturer is Becton-Dickinson (BD), A BD spokesperson said that during Covid, they have seen “the most unpredictable demand that BD has experienced in our company’s history.” They added, “Worldwide, BD produced nearly a half a billion additional blood tubes in 2021 versus 2020, The shortage was first found in the light-colored lavender tubes that are used for assessing a patients coagulation. Since many covid patients are at risk for blood clots these tubes ran out first. “
Worldwide labor shortages, raw material shortages and shipping delays are hindering the supply of these tubes, with no end in sight.
Because of this the FDA is recommending rationing these tubes for necessary, urgent cases and not for routine screenings.
This has left many people without necessary preventative and routine testing.
As stated, there is no end to the shortage in the immediate future.
History of Vacutainers
Vacutainer tubes in glass were invented by Joseph Kleiner in 1947. The plastic version, known as Vacutainer PLUS, was developed at Becton Dickinson Research Center during 1991-1993, by co-inventors E. Vogler, D. Montgomery and G. Harper.
Prior to the invention of an evacuated tube system, before collecting blood, solutions for the additive tubes like EDTA and citrate were prepared and dispensed into test tubes for blood anticoagulation. Then, to identify the proper draw volume, the laboratory used to etch lines in the borosilicate glass tubes. The phlebotomist would collect blood specimens with needles and glass syringes. After collection, the blood would be transferred into a series of test tubes and sealed the tubes with black rubber stoppers for transportation of the specimens to the laboratory. For electrolyte measurements, mineral oil was added to the tubes to prevent loss of CO2. For serum specimens, wooden applicator sticks were used to loosen the clot from the tube walls .
The shortcomings of these techniques were numerous. The patients were subjected to the ordeal of multiple needle entries to the vein. The errors during the collection and transfer process and the safety risks were unavoidable
The introduction of vacuum blood collection systems marked an era of greater safety, easy handling, speed, and accuracy in blood-to-additive ratios. Initially during blood collection with evacuated tubes, one end of the needle entered the patient’s vein; the other end penetrated the rubber stopper as the tube was pushed into the open end of the holder. The vacuum enabled the tube to fill with the appropriate volume of blood.
Now, there are regulatory agencies and guidelines that ensure the consistency in the design and manufacture of blood collection systems like Food and Drug Administration (FDA); International Standardization Organization (ISO); and Clinical Laboratory Standards Institute (CLSI); The Medical Device Amendment (1976) and the Safe Medical Devices Act (1990).
Alternative to vacutainers

Alternatives to vacutainers have been around for many years. They have a proven track record and could fill the gap the widely used but in short supply that vacutainers are facing. Prothombin times and INR (PT/INR) coagulation tests use the light lavender topped vacutainers that were initially put on the vacutainer shortage list.
At home devices, like the standard glucometer testing devices widely used to test blood glucose levels at home, can allow a patient to take this test in the comfort of their home using a very small sample of blood. Called the LabPad INR machine, Avalun technologies has developed a handheld device that can read a patients PT/INR in a matter of minutes using a small blood sample obtained by a fingerpick.
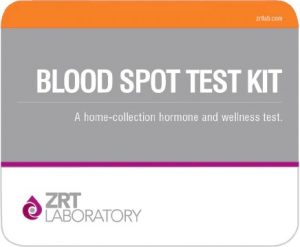
Dried Blood Spot testing
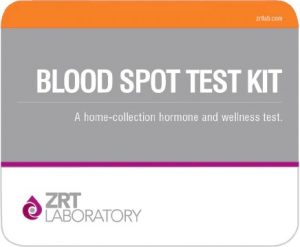
Dried blood spot testing (DBS) has been a widely accepted form of testing for years. A fingerpick of blood is placed on a specially prepared absorbent paper and allowed to dry. The sample is sealed and usually put in the mail or hand carried to the laboratory. One company, ZRT labs use this form of testing for a wide number of tests, from hormone tests such as thyroid, insulin, female and male hormones, drug screening, heavy metals, cholesterol and many more tests. Along with the LabPad INR machine this type of testing could free up many vacutainers and help curb the shortage.
Manufactured in US, a global company offers microsampling solution

Another form of testing offered through a US based company called Neoteryx, offers microsampling of blood for a wide variety of labs.
According to their press information sheet:
Neoteryx is a medical device company that researches, develops, and manufactures microsampling devices for the remote collection of blood and other bio-fluids. Their flagship device, the Mitra® Microsampler is a simple, convenient alternative to traditional, phlebotomy-based blooddraws that delivers high quality, precise samples for laboratory analysis.
Mitra microsamplers can be used by anyone, anywhere, virtually eliminating the need for most clinic-based blood draws. By taking blood collection out of the clinic, Neoteryx is enabling patient-centered telemedicine and supporting virtual studies in research science. The Mitra® device, based on VAMS® our patented volumetric microsampling technology, is a specimen collection breakthrough. It combines the best of traditional blood sampling, dried blood spot cards and microsampling technology into an easy-to-use, remote specimen collection device.
Mitra has applications in drug research, clinical trials, precision medicine, patient-centered care, and public health studies that reach underserved regions and beyond.”
Of interest is that this company manufactures and is based out of the United States, however it is only available for use in the US for research projects.
According to the small print at the bottom of their website: “They are CE-IVD self-certified in the UK and EU, a Class 1 IVD in Australia, Brazil & China, Class B in South Africa, and registered with health agencies in Canada, Thailand, and Ukraine. In the United States, Mitra devices are for Research Use Only (RUO). “
Given the severe shortage of blood collection tubes, hopefully these devices will be released for use past research in the country they are manufactured, namely the United States very soon.
I contacted the spokesman, David Norris for GE Healthcare, the primary producer of the iodine based contrast dye that is used in CT scans and other Xray applications, and he sent a press release posted June 2,2022,
“GE Healthcare expects production capacity from its Shanghai facility to be close to 100% starting next week (Monday 6 June), following the easing of local COVID restrictions. This will enable us to restabilize our global supply of iodinated contrast media. We will continue to work with impacted customers to help them plan several weeks ahead as supply progressively recovers.”
GE Healthcare has 4 contrast dye facilities and had increased production in its factory in Ireland and has been shipped via air to offset the shortage, however the supply accounts for a very small percentage of the contrast dye used.
This is encouraging news for all the people that have had tests canceled and had forgone routine testing.
Contrast Media recycling Pilot Program Going Well
As far as the contrast media recycling program mentioned in the previous post, according to GE Healthcare representative David Norris, the recycle program for contrast media in the US is going well at the pilot site. Advocate Aurora Health is a leading hospital group with 26 hospitals throughout Illinois and Wisconsin performed 20,000 contrast media studies in 2021. They are currently part of the pilot program and so far, it seems to be a success, according to Joannah Ludwig, imaging manager at Advocate Aurora Health.
How it works: The recycling program provides the imaging and radiology departments with 3-liter bottles which are filled with uncontaminated and unused contrast media, sealed, and shipped back to their recycling plant in Lindenses, Norway. The dye is processed and used to produce more contrast media. The program is expected to roll out nationwide in the US by the end of this year. This program has been in effect in Europe since 2006, and in Canada since last year where 15 hospital complexes are involved.
Given the fact that iodine is not a renewable resource, recycling this product will be a vital part of our healthcare system until another form of media is found to be as effective.
In the United States 40% of all CT scans use contrast media, and worldwide only 18% of the iodine-based contrast media is reused.
Logistics and the medical infrastructure

One of the roadblocks we are facing in all sectors of the economy is the logistical nightmare of getting any product from manufacture to its destination. The blocked ports and decreased supply due to lockdowns only paint a limited picture of why medications and medical supplies are in short supply. Once the product is delivered to the States it is subject to many regulations and laws surrounding the import of goods into our country. Along with the increasing rise of diesel and shortage of DEF (Diesel Exhaust Fluid) that is used in trucks there are increasing numbers of truckers that are concerned about the cost of driving product to its destination Some small trucking companies are at risk of shutting down altogether. This would put a strain on our already overwhelmed infrastructure.
Be Prepared the World is rapidly changing

We are in a state of emergency with all sectors of our commerce, travel, healthcare, food, and energy in dire straights. It may just seem like an inconvenience now; however, our entire way of life is changing before our eyes. Don’t get caught unprepared. What used to be considered normal human behavior- stocking up for a rainy day- is now being criticized and labeled a hoarder. Don’t let these labels keep you from doing what you know is the right thing to do. Being able to help your family, loved ones and neighbors with time and resources and not having to depend so much on our failing infrastructure is being a part of the solution, not part of the problem.

While our healthcare system is still intact and functioning take time to get your medical needs, labs and any medications refilled and stored. If this all blows over and we are finding ourselves with extra food, up to date dental and medical needs we will be that much more ahead.
Don’t be overwhelmed, just take 1 small step each day to ensure you and your loved one’s health, food, shelter and emotional needs are met as we enter this new world we are finding ourselves in.
Reports through the nation’s hospitals are sharing stories of severe shortages of medicines, IV solutions, durable medical equipment and contrast dyes used in diagnostic procedures. The situation is dire and isn’t getting any better soon.
Supply shortages include
- Dialysis supplies
- Laboratory testing reagents and testing supplies
- Vinyl examination gloves and surgical gowns
- Ventilator related products
- Contrast dyes for CT and MRI procedures
How are supply shortages determined?
The CARES act of 2020
According to the FDA:
The Coronavirus Aid Relief and Economic Security Act(CARES Act) was signed into law on March 27.2020 to aid response efforts and ease the economic impact of COVID-19. In addition, the CARES act authorized the FDAs ability to identify, prevent and mitigate possible shortages of drugs and medical product supply chains. Drug shortages can occur for various reasons, including manufacturing and quality problems, delays, and discontinuations. Drug manufacturers provide FDA with most of the drug shortage information the agency receives, and the agency works closely with manufacturers to prevent or reduce the impact of shortages. This has proven to be a tremendous help in identifying potential drug and medical supply shortages and possible future shortages. Even with this act in place we are experiencing historic shortages that the cause of is out of our control.

Logistics, Lockdowns and Backlogged
The ongoing health crisis has prevented the manufacture and flow of medical supplies worldwide. Backlogged ports, lockdowns in China, ingredients to manufacture drugs and supplies are all impacted. Hospitals and medical facilities around the United States have been dealing with disruptions and in some cases out of stock medications and supplies. Many hospitals are reporting they have had to ration procedures and supplies to extreme, lifesaving emergencies. Raw materials for many drugs that are sourced from India and shipped to China to manufacture the medications are unable to ship their material to China due to the ongoing lockdowns and port closures in China.
This situation could turn very dire this summer if restrictions and lockdowns continue. Shutdowns have yet to fully work their way through the supply chain, meaning that constrained supplies could get worse this summer, especially if the lockdowns drag on.
Supply logistics are another problem. Once the supplies and drugs arrive at the US ports they still must be shipped across the country to hospitals, clinics, and other healthcare facilities. The diesel shortage and skyrocketing cost of diesel are playing a huge part in this lag time.
These shortages are expected to impact our healthcare facilities, and ultimately us, the patients well into 2023.
A look at critical supply shortages
Over the next weeks we will be exploring the different medical supply shortages affecting healthcare facilities in the United States, beginning with contrast media.

Contrast media for CT studies and imaging.
Iohexol- trade name Omnipaque
This is an iodine-based contrast dye widely used in CT scans and x rays, such as kidney, heart, urinary tract, GI tract and spine. It belongs to a class of drugs known as contrast media or dyes. It works by adding contrast to body parts and fluids in imaging tests, allowing the doctor to see abnormalities or changes in a patient’s condition. About 40% of all CT scans use contrast media.
Contrast media has been rationed and hospitals and healthcare facilities have been asked to only use in the most emergent cases. This has led to cancellation of exploratory and routine CT and Xray procedures.
According to a statement from the AHA website:
Nancy Foster, AHA’s vice president for quality and patient safety policy, said, “We are aware of this global shortage of IV contrast fluid due to production shutdowns in China and have raised this issue with the Administration. While we have been told to expect normal production to resume late next month, hospitals are exploring various conservation strategies including the use of other imaging technologies, using other contrast agents, rationing contrast, and ensuring every available drop of contrast dye is used efficiently, and postponing some scans that can be postponed, to give a few examples, to continue to provide needed care. The AHA will continue to monitor this situation and provide updates to the hospital and health system field.”
GE Healthcare reports on restarting production of Omnipaque:
“The impacted facility (in Shanghai) had increased production output from 0% of capacity when the plant was closed to 60% by May 21, 2022. GE Healthcare expects the plant to be producing at 75% in the next two weeks.” In addition, they are expanding production in their Cork, Ireland facility. They are projecting more contrast dye will be available by June 30tj.
Recycling unused contrast media program
In the meantime, however, there remains a severe shortage of Omnipaque. GE healthcare has been recycling iodine-based contrast media left over from procedures since 2006 in 11 European countries and since spring of 2021 has expanded its service to the United States and Canada. Canada currently has 15 collection sites, and as of this writing, the United States is in the exploratory phase to implement this program
Taking personal responsibility for your health
As we continue to experience supply chain shortages in the most critical sector of our lives, mainly the healthcare industry, it would be a good time to assess you and your loved one’s medical readiness at home, and to take preventative steps towards health, such as nutrition, stress reduction, exercise and nurturing close relationships.
In addition, it would be a good time to go through your medicine chest and discard out of date medications, stock up on first aid supplies that you may be running low on, and to renew your prescription medications.

Reports of Monkey Pox are in the headlines now, from case fatality rates as high as 10 percent to the virus being part of a planned bioterror attack.
A few recent headlines:
British officials confirm 19 more monkeypox cases
Monkeypox spread “concerning” say President Biden
Third possible case of monkeypox found in US
WHO asks for ‘strengthened coordination’ as monkeypox outbreak reaches the US
To sort out fact from sensational headlines below are some statistics and facts taken from the World Health Organization and CDC:
About Monkeypox:
Monkeypox is a rare disease that is in the same genus as smallpox and cowpox. Monkeypox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, hence the name ‘monkeypox.’ The first human case of monkeypox was recorded in 1970 in the Democratic Republic of the Congo (DRC) during a period of intensified effort to eliminate smallpox. Since then, there have been small outbreaks throughout the world, The first outbreak in the US was in 2003 when 71 individuals were infected following sale of prairie dogs infected with Gambian giant rats that had been imported from Ghana. They had been housed in the same facility for an extended time and became infected. Since then, there has been isolated outbreaks in the United States.
About the monkeypox virus
There are two clades of monkeypox virus: the West African clade and Congo Basin (Central African) clade. Although the West African clade of monkeypox virus infection sometimes leads to severe illness in some individuals, disease is usually self-limiting. The case fatality ratio for the West African clade has been documented to be around 1%, whereas for the Congo Basin clade, it may be as high as 10%. Children are also at higher risk, and monkeypox during pregnancy may lead to complications, congenital monkeypox or stillbirth.
On May 6th, 2022, the first laboratory confirmed case of West African monkeypox in a UK resident returning from a visit to Delta and Lagos in Nigeria. Since then, there have been reports of the virus in Europe (e.g., England, Portugal, Spain, Sweden, Italy, Belgium, France), North America (e.g., United States, Canada) and Australia. Some cases were reported among men who have sex with men. Some cases were also reported in people who live in the same household as an infected person.
None of these people reported having recently been in central or west African countries where monkeypox usually occurs, including the Democratic Republic of the Congo and Nigeria,
The current outbreak appears to be the less severe form of monkeypox- the West African monkeypox virus.
Facts taken from the CDC website on monkeypox:
- Monkeypox is less contagious than smallpox and causes less severe illness.
- Transmission is from one person to another by close contact with lesions, body fluids, respiratory droplets and contaminated materials such as bedding or clothing.
Incubation period
Infection with monkeypox virus begins with an incubation period. A person is not contagious during this period.
- Incubation period averages 7−14 days but can range from 5−21 days.
- A person does not have symptoms and may feel fine.
Monkeypox symptoms usually happen in two stages.
- The first stage includes
- fever, headache
- , muscle aches
- , swollen lymph nodes,
- and exhaustion.
- One to three days after the fever starts, a rash appears.
The second stage begins with the rash that starts on the face before spreading to other parts of the body.
- The first lesions to develop are on the tongue and in the mouth.
- Within 1-2 days a macular rash appears on the skin, starting on the face and spreading to the arms and legs and then to the hands and feet, including the palms and soles.
- The rash typically spreads to all parts of the body within 24 hours becoming most concentrated on the face, arms, and legs (centrifugal distribution).
- By the third day of rash, lesions have progressed from macular (flat) to papular (raised).
- By the fourth to fifth day, lesions have become vesicular (raised and filled with clear fluid).
- By the sixth to seventh day, lesions have become pustular (filled with opaque fluid) – sharply raised, usually round, and firm to the touch (deep seated).
- Lesions will develop a depression in the center (umbilication).
- The pustules will remain for approximately 5 to 7 days before beginning to crust.
- By the end of the second week, pustules have crusted and scabbed over.
- Scabs will remain for about a week before beginning to fall off.
- Pitted scars and/or areas of lighter or darker skin may remain after scabs have fallen off. Once all scabs have fallen off a person is no longer contagious.

Vaccination
Since monkeypox and smallpox are very similar the smallpox vaccine is considered effective to prevent monkeypox.
ACAM200 and JYNNEOSTM (also known as Imvamune or Imvanex) are the two currently licensed vaccines in the United States to prevent smallpox. JYNNEOS is also licensed specifically to prevent monkeypox. You are not considered fully vaccinated until you receive 2 doses of the vaccine.
Vaccination after exposure
CDC recommends that the vaccine be given within 4 days from the date of exposure in order to prevent onset of the disease. If given between 4–14 days after the date of exposure, vaccination may reduce the symptoms of disease, but may not prevent the disease. Persons exposed to monkeypox virus and who have not received the smallpox vaccine within the last 3 years, should consider getting vaccinated.
The sooner the person receives the vaccine, the more effective it will be in protecting against monkeypox virus.
In conclusion
At his point there seems to be no real threat to contracting monkeypox unless you have been directly exposed to someone who has a confirmed case, or you have traveled to an at-risk nation/region. There are vaccinations with an 85% success rate available, and the US has enough supply of vaccines for now. Always consult your primary health practitioner for guidance.
As parents desperately search from store to store, city to city and even reports of state to state for baby formula we are left with some questions:
When and where did the formula shortage start?
Back in February, Abbott Laboratories initiated a recall of powdered infant formula produced at its Sturgis, Michigan, facility, after receiving reports of bacterial infection in several babies. Similac 60/40 PM was the first formula to be recalled after two infants died after ingesting the formula that carried the bacteria Cronobacter sakazakii. The Similac PM 60/40 recall is in addition to other lots of Similac, Alimentum, and EleCare powdered formula that were recalled on February 17, 2022, for possible Cronobacter contamination.
By May 8th there was a 43% shortage of formula across the U.S.
There are only 4 companies that produce formula in the States. The reason being is there are extensive regulations and inspections surrounding the production of baby formula. According to data compiled by Allied Market Research, four companies control about 90% of the U.S. infant formula industry:
- Abbott Nutrition
- Mead Johnson Nutrition
- Nestle USA
- Perrio Company

What is the pathogen that has contaminated the formula and how does it infect?
Cronobacter sakazakii is a bacterium that causes a rare but often fatal infection of the bloodstream and central nervous system. Infants with weakened immune systems, particularly premature infants, are most likely to contract an Cronobacter infection, although the bacteria have caused illnesses in all age groups. What makes this bacteria so dangerous is that it can live in dry conditions for over 2 years. This bacteria caused a recall of tampons in 2011.

When will the supply be replenished and up and running?
The FDA has reached an agreement with Abbot to reopen their formula making facility. They will require a third-party expert at the facility to assure the formula is made safely. A spokesman for the facility has stated it will take between 6 and 8 weeks before formula will be available on grocery shelves.
In the meantime, the White House reports that it has launched Operation Fly Formula. The Department of Defense will use its contracts with commercial cargo airlines to transport products from manufacturing facilities abroad that have met Food and Drug Administration safety standards.
Also, Nestle is flying formula in from Netherlands and Switzerland to combat the formula shortage.

Why not just make your own formula?
Infant formula shortage has led to some parents attempting some desperate measures. One ER physician recounts parents feeding their infants diluted formula, leading to sodium deficiencies. This has led to some babies having a depleted fluid volume, resulting in a dangerously low blood pressure and low circulating oxygen volume. Electrolyte balances in infants is very dangerous. Their bodies, being small and still developing cannot cope with electrolyte depletion as compared to older children and adults. In extreme cases these imbalances can lead to seizures.
Some online advice advocates feeding cow’s milk to infants who are under 12 months of age. According to the American Association of Pediatrics for babies older than 6 months, cow’s milk is an option “for a brief period of time” but the AAP cautions it “should not become routine” due to concerns infants won’t get enough iron.
You should not make your own formula using a recipe found online or elsewhere, according to the FDA and the AAP. Homemade formulas can be dangerous, leading to contamination and low calcium, the FDA says. Reports of infant deaths using homemade formulas have been reported.
Available Resources
- Check with your baby’s pediatrician for any available sources of formula and if it is ok to switch formulas if necessary. Your babys doctor know what is best for your baby.
- In addition, ask your pediatrician if there are any goats milk formulas that would work
- Check online sources, such as larger online stores that may have formula available. Only purchase from well recognized distributors
- Check social media groups, local WIC offices, parents groups for any available formula.
- Contact the Human Milk Bank of America for guidance
- Locate your local Community Action Association for assistance
- In some instances, if breastfeeding had been discontinued, the La Leche league states that it may be possible to restart breastfeeding, also known as relactation. This would require time, patience, determination, and a cooperative baby, according to their website
Manufacturer Hotlines
- Gerber’s MyGerber Baby Expert : reach a certified nutrition or lactation consultant by phone, text, Facebook Messenger, web chat, or video call, who can help you identify a similar formula that may be more readily available
- Abbott’s Consumer Hotline: call 1-800-986-8540
- Abbott’s urgent product request line : ask your OBGYN or your infant’s pediatrician to submit an urgent product request by downloading and completing the form – PDF
- Reckitt’s Customer Service line: call 1-800 BABY-123 (222-9123)
Hopefully the formula shortage will be short lived. In the meantime, utilize the above resources to help you find the formula your infant needs. For future reference, once formula is available it is NOT hoarding to buy extra formula and put it away. Just like stocking extra food for the upcoming food shortage our government is telling us about, your infants food supply is a priority.