Its tick season, Are you ready?
Its that time of year again. Along with lovely, warm, sunny days, gardens in full production, Long walks along winding paths through the woods comes the emergence of the dreaded tick. Honestly, I haven’t found ticks to be of much good use other than food for birds, frigs, spiders and other animals. They carry many disease and can be difficult to find on the body.
Although ticks are commonly thought of as insects, they are arachnids like scorpions, spiders and mites. Ticks are among the most efficient carriers of disease because they attach firmly when sucking blood, feed slowly and may go unnoticed for a considerable time while feeding.
There are two types of ticks that infect humans. The first is the Ixodidae, known as the hard tick. This tick is the most common tick that bites and infects humans. The other is the Argasidae, known as the soft tick.
Where are ticks found

Ticks are usually found outdoors in wooded and grassy areas but are also found in cabins, woodpiles, and caves. They can even be found on your dog after a romp through the grass!
They way ticks find their next meal/host is by detecting the animal’s breath and body odors, by sensing bod heat, moisture, and vibrations. They wait for a host by resting on the tips of grasses and shrubs along well traveled paths. Since they can’t fly or jump, they rest on the tips of grasses or shrubs in a position known as “questing/ From there the ticks latch on to its host.
How ticks spread disease
Some ticks will attach quickly, and others will wander, looking for places like the ear, or other areas where the skin is thinner.
- Depending on the tick species and its stage of life, preparing to feed can take from 10 minutes to 2 hours. When the tick finds a feeding spot, it grasps the skin and cuts into the surface.
- The tick then inserts its feeding tube. Many species also secrete a cement-like substance that keeps them attached during the meal. The feeding tube can have barbs which help keep the tick in place.
- Ticks also can secrete small amounts of saliva with anesthetic properties so that the animal or person can’t feel that the tick has attached itself. If the tick is in a sheltered spot, it can go unnoticed.
- A tick will suck the blood slowly for several days. If the host animal has a bloodborne infection, the tick will ingest the pathogens with the blood.
Many ticks go through life cycles that can span 3 years and go between different hosts. In this way they can widely spread disease between hosts.
Common tickborne diseases
Ticks can be infected with bacteria, viruses or parasites. Some of the most common tick-borne diseases in the United States include: Lyme disease, babesiosis, ehrlichiosis, Rocky Mountain Spotted Fever, anaplasmosis, Southern Tick-Associated Rash Illness, Tick-Borne Relapsing Fever, and tularemia. Other tick-borne diseases in the United States include: Colorado tick fever, Powassan encephalitis, and Q fever.
Lyme disease is probably the most well known tickborne disease, however there are several other diseases that ticks carry. For instance, the Lone Star tick can carry Heartland virus which can cause severe illness and even death. The Lone Star tick also can cause an allergic reaction called alpha gal syndrome which causes the host to become allergic to red meat.
| Pathogen | Disease | States | Counties |
| Borrelia burgdorferi | Lyme disease | 30* | 476 |
| Borrelia miyamotoi | Hard tick relapsing fever | 25* | 271 |
| Anaplasma phagocytophilum | Anaplasmosis | 24* | 291 |
| Babesia microti | Babesiosis | 17 | 154 |
| Powassan virus | Powassan virus disease | 6 | 55 |
| Borrelia mayonii | Lyme disease | 4 | 12 |
| Ehrlichia muris eauclairensis | Ehrlichiosis | 2 | 11 |
Lyme Disease
The most widely known and reported tickborne disease that is most likey very underreported is Lyme disease:- approximately 30,000 cases are reported every year, however insurance statistics put the yearly total at more than 476,000 cases that are diagnosed and treated every year.
Lyme disease can be treated effectively with a single dose of doxycycline if diagnosed soon after bitten. (Note that the Jase case is equipped with doxycycline as one of the five antibiotics) If treatment is delayed, Lyme disease can manifest in many debilitating diseases, such as arthritis, facial paralysis, rashes, fevers.
Initial rash of Lyme disease (Erythema Migrans rash) is caused by the bacterium Borrelia burgdorferi and rarely, Borrelia mayonii.
Below is an image of early stages of the rash. More information can be found on the CDC website under Lyme disease.

Prevention of Tick-Borne diseases
There are so many different diseases that are caried by ticks, that many health practitioners aren’t aware of all the diseases and symptoms. It would be almost impossible for your health practitioner to know each tick exposure and associated diseases. It is the responsibility of the individual to know the common ticks and diseases they may carry when venturing outdoors. The CDC has an extensive website on disease causing ticks.
Prevention- avoid exposure: taken directly from the CDC website:
Tick exposure can occur year-round, but ticks are most active during warmer months (April-September). Know which ticks are most common in your area.
Before You Go Outdoors
Know where to expect ticks. Ticks live in grassy, brushy, or wooded areas, or even on animals. Spending time outside walking your dog, camping, gardening, or hunting could bring you in close contact with ticks. Many people get ticks in their own yard or neighborhood.
Treat clothing and gear with products containing 0.5% permethrin. Permethrin can be used to treat boots, clothing and camping gear and remain protective through several washings. Alternatively, you can buy permethrin-treated clothing and gear.
Use Environmental Protection Agency (EPA)-registered insect repellents containing DEET, picaridin, IR3535, Oil of Lemon Eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. EPA’s helpful search tool can help you find the product that best suits your needs. Always follow product instructions. Do not use products containing OLE or PMD on children under 3 years old.
Avoid Contact with Ticks
Avoid hiking through wooded and brushy areas with high grass and leaf litter. Walk in the center of trails. Keep lawns mowed, weeds to a minimum in the yard.
After You Come Indoors
Check your clothing for ticks. Ticks may be carried into the house on clothing. Any ticks that are found should be removed. Tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors. If the clothes are damp, additional time may be needed. If the clothes require washing first, hot water is recommended. Cold and medium temperature water will not kill ticks.
Examine gear and pets. Ticks can ride into the home on clothing and pets, then attach to a person later, so carefully examine pets, coats, and daypacks. Consider tick preventative medication or collars for your pets.
Shower soon after being outdoors. Showering within two hours of coming indoors has been shown to reduce your risk of getting Lyme disease and may be effective in reducing the risk of other tickborne diseases. Showering may help wash off unattached ticks and it is a good opportunity to do a tick check.
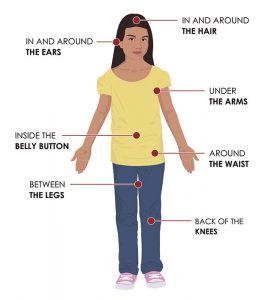
Check your body for ticks after being outdoors. Conduct a full body check upon return from potentially tick-infested areas, including your own backyard. Use a hand-held or full-length mirror to view all parts of your body. Check these parts of your body and your child’s body for ticks:
- Under the arms
- In and around the ears
- Inside belly button
- Back of the knees
- In and around the hair
- Between the legs
- Around the waist
Create a tick safe zone to reduce or eliminate ticks in your backyard.
From the CDC website:
The Connecticut Agricultural Experiment Station has developed a comprehensive Tick Management Handbook for preventing tick bites. Here are some simple landscaping techniques that can help reduce blacklegged tick populations:
- Remove leaf litter.
- Clear tall grasses and brush around homes and at the edge of lawns.
- Place a 3-ft wide barrier of wood chips or gravel between lawns and wooded areas to restrict tick migration into recreational areas.
- Mow the lawn frequently.
- Stack wood neatly and in a dry area (discourages rodents).
- Keep playground equipment, decks, and patios away from yard edges and trees.
- Discourage unwelcome animals (such as deer, raccoons, and stray dogs) from entering your yard by constructing fences.
- Remove old furniture, mattresses, or trash from the yard that may give ticks a place to hide.
Essential oils as tick repellant
A word about essential oils and their efficacy in acting as a tick repellent:
There are many claims about essential oils used as an effective tick repellant on the internet. Some point to studies done on selected ticks and make claims that these oils are just as effective as DEET. Cedarwood, cinnamon, lemon eucalyptus, oregano oil(this oil was the most effective) and other oils have demonstrated a level of repellant qualities, however they must be applied ever few hours and are not as effective as DEET. . Most of these claims are somewhat correct, however they are not as effective as DEET.
How to remove a tick
The following is directly from the CDC website on tick removal, they have a “tick bot” that can guide you through the process of safely removing the tick if you should happen to find one embedded in your skin.

Use clean, fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible.
Pull upward with steady, even pressure. Don’t twist or jerk the tick; this can cause the mouthparts to break off and remain in the skin. If this happens, remove the mouthparts with tweezers. If you cannot remove the mouth easily with tweezers, leave it alone and let the skin heal.
After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.
Never crush a tick with your fingers. Dispose of a live tick by
- Putting it in alcohol,
- Placing it in a sealed bag/container,
- Wrapping it tightly in tape, or
- Flushing it down the toilet.
Follow-up
If you develop a rash or fever within several weeks of removing a tick, see your doctor:
- Tell the doctor about your recent tick bite,
- When the bite occurred, and
- Where you most likely acquired the tick.
- Avoid folklore remedies such as “painting” the tick with nail polish or petroleum jelly, or using heat to make the tick detach from the skin. Your goal is to remove the tick as quickly as possible–not waiting for it to detach.
