A highly concerning survey conducted by the Pharmacy Technician Certification Board, who grants a Supply Chain and Inventory Management for certification, has stated that nearly 96% of respondents report the pharmacy they work for faces drug shortages. Established in...
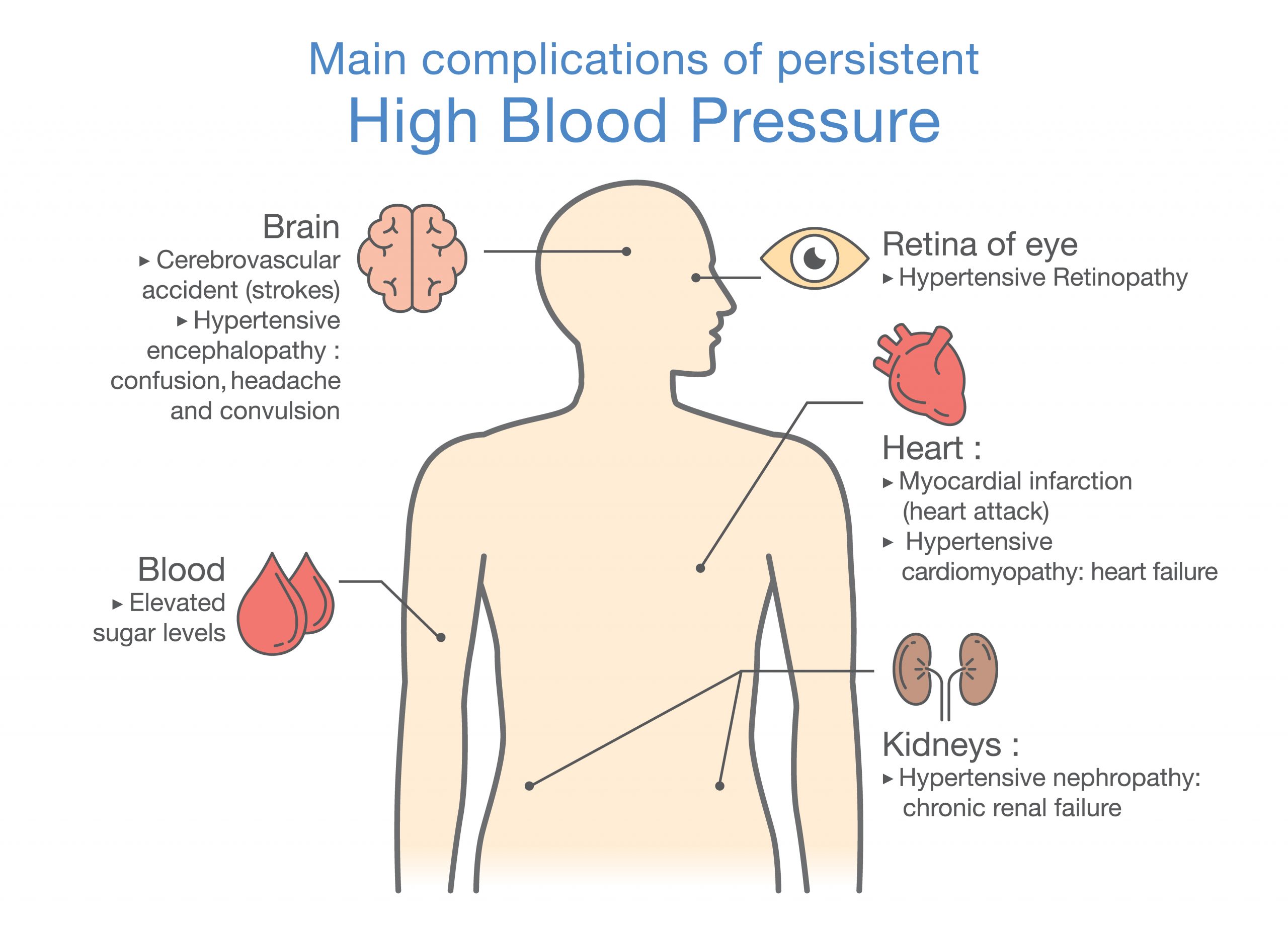
The Silent Killer (Part 3)

The silent killer, aka hypertension can be controlled, even prevented by making some simple lifestyle changes. Below are some of the most effective ways to increase your health while decreasing your blood pressure. This may reduce or eliminate your need for medication, along with reducing your r
- Nutrition

There are many nutritional approaches to reduce blood pressure, probably the most famous, is the DASH diet (Dietary approaches to stop hypertension) promoted by the National Heart, Lung and Blood institute, a branch of the National Institute of health, this diet plan has a proven track record of lowering blood pressure. According to the NHLBI website:
“The DASH eating plan requires no special foods and instead provides daily and weekly nutritional goals. This plan recommends:
- Eating vegetables, fruits, and whole grains
- Including fat-free or low-fat dairy products, fish, poultry, beans, nuts, and vegetable oils
- Limiting foods that are high in saturated fat, such as fatty meats, full-fat dairy products, and tropical oils such as coconut, palm kernel, and palm oils
- Limiting sugar-sweetened beverages and sweets
- When combined with a low sodium diet, the DASH diet was even more effective at lowering blood pressure. For more information on the Dash diet, check our this website.
- Add citrus, especially grapefruits, lemons, limes, and oranges. They also fight cancer. A recent study revealed that when grapefruit and beetroot juice are combined, they provide a synergistic effect on systolic (top number, when blood is pumped through the system) which lowered blood pressure. Beetroot juice contains nitrites, Nitrites are widely known to relax blood vessels, which lowers blood pressure. Grapefruit juice contains an ingredient that allows nitrite to be more available for the body in a complex process that inhibits reoxidation of nitrite to nitrate.
2. Lose weight, if needed
Portion size and calorie reduction are effective weight loss strategies. In addition, there are many online and in person programs that can help with your weight loss journey. Some popular ones are:
- Noom- This is an online interactive weight loss program that deals with psychology of eating along with health food choices. It is highly rated (9.8/10)and has earned the top weight loss plan off 2023 by
- Weight watchers has in person and online programs. This time-tested program is still effective and popular.
- Premade delivered to your door meals. Premade delivered meals have blossomed into a very popular way to combine the convenience of healthy foods with portion control. Meal delivery services offer diet and heart healthy menus. Some of the more popular meal delivery services are Factor, Hello Fresh, and Nutri System.
3. Get a dog – or any pet
Spending time with a pet, whether is a dog, cat or any other animal can help alleviate stress (one leading cause of hypertension) and promote improved mental wellbeing.
- Dog owners are more likely to take their furry animals on a walk. Regular exercise is widely regarded as a way to lower blood pressure and overall improve cardiovascular health.
- Petting, talking, or interacting with your dog or cat significantly lowers blood pressure according to research.
- Pets provide companionship especially if living alone or have few social contacts. Of note, Older women are more likely than men to experience hypertension when socially isolated.
4. Community involvement
Being part of an active community has proven health benefits, including lower blood pressure, increased heart, and emotional health.
Friends, family, neighbors, social clubs, volunteer, and religious communities can offer the connectiveness and belonging, bringing meaning to our lives. Having a strong support system- having someone to call when in need- alleviates stress, which in turn lowers blood pressure.
5. Breathe – and meditate
One of the most underrated ways to reduce blood pressure that is free and anyone can do are breathing and meditation exercises.
- A study done out of University of Colorado, Boulder revealed that a 5 minute, 6 days a week breathing program lowered systolic blood pressure by 9mm hg, This technique, called High-Resistance Inspiratory Muscle Strength Training (IMST) was originated in the 1980s way to help critically ill respiratory disease patients strengthen their diaphragm and other inspiratory (breathing) muscles, IMST involves inhaling vigorously through a hand-held device which provides resistance. Imagine sucking hard through a tube that sucks back. In addition to lowered blood pressure, this 30-breath technique could also improve cognitive function as well.
- Meditate- 20 minutes once a day has also been a time honored and proven method to improve both systolic and diastolic blood pressure markers. Mindfulness based meditation , has been shown to have a temporary effect on both systolic and diastolic blood pressure.
In addition, people that practice meditation-prayer on a daily basis are less likely to need blood pressure medication.
Along with the above recommendations, getting a good night’s sleep, limiting (less than 1 drink for women, 2 drinks for men per day) alcohol and stopping smoking (known to raise blood pressure) are all natural ways to help control blood pressure.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
Pharmacy Techs Report Massive Drug Shortages
The Largest Strike in Healthcare Workers Begins Tomorrow – Are You Ready?
Citing unfair labor practices and overworked staff, the Coalition of Kaiser Permanente Unions, Kaiser Permanente healthcare workers will be striking for 3 days, starting Oct. 4 at 6 am through 6 am, Oct. 7, 2023. 75,000 Kaiser healthcare workers from California,...
Emergency Alert – Rural Hospitals Closing at an Alarming Rate
You will need to be your own first responderAccording to the Center for Healthcare Quality and Patient Reform, around 30% of all rural hospitals in the U.S. are at a risk of closure due to financial issues. It is expected that these losses will likely increase as...