If no medical care is available-Do all members of your family have a Jase Case? Melissa Gilbert of Little House on the Prairie, recently posted on Instagram that she had to go to the hospital. 2 days prior, an insect bit her arm. The bite had turned red, swollen, and...
3 Common Back to School Illnesses Part 1 of 2

Part 1
As summer winds down, children across the nation are returning to school. Whether in public school or homeschooled they will be exposed to more germs as they interact with their peers.
Children aren’t exempt from the annual onslaught of germs. Every year teachers and those who work with children end up with colds, flu and other common illnesses that the new school year brings.
Let’s take a look at 3 common back to school illnesses.
- Colds, flu and coronavirus
Colds, flu and coronavirus are all highly contagious and can be almost impossible to avoid. Luckily these illnesses are usually not life threatening and can be managed with symptomatic treatment.
If your child is in a high-risk category, be sure to contact your primary care provider for guidance and follow their recommendations on vaccination and other preventative measures.
To build up and help fight these viruses:
- Get adequate sleep. Especially during the school year, a set schedule is very important. Sleep is where your body repairs and heals.
- Avoid sugar. Sugar brings the immune system down.
- Eat plenty of fresh or frozen vegetables and fruits. At least 4-6 servings a day.
- Vigorously wash hands in soapy water for 30 seconds.
- Sneeze and cough into crook of elbow, or tissue. Discard tissue and wash hands.
- Fresh air and exercise outside, weather permitting. This helps build up the immune system.
Treatment
Many viruses run their course. They provide immunity in the form of antibodies to help combat further exposure to the virus.
To alleviate discomfort associated with viruses:
- Try over the counter or prescription decongestants, expectorants, cough suppressants and pain relivers as recommended by your primary care provider.
- Studies on honey as a cough suppressant have been encouraging. Honey with lemon or tea has been a time-honored treatment for sore throats and cough.
- Diffusers with essential oils such as mint or eucalyptus can help breathing and congestion.
- A cool mist humidifier can provide relief.
- Be sure to stay hydrated, especially if running a fever.

2. Head lice (not an illness, however they are common and pesky!)
Head lice are tiny insects that feed on blood from the scalp. They cannot jump or fly and are passed from person to person via direct contact, either from close contact with someone who has lice or sharing combs, brushes, clothing (hats, hoodies, coats)
Identify: If there is an infestation, all household members need to be inspected for lice. Because adult and nymph lice are very small, move quickly, and avoid light, they may be difficult to find. Use of a fine-toothed louse comb may facilitate identification of live lice. Nits (nits are
the empty egg cases attached to hair that head lice hatch from)
Nits frequently are seen on hair behind the ears and near the back of the neck.
Many times, dirt, dust and dander can look like lice and can be misdiagnosed.

Treatment:
Whether using an over the counter or prescription medication to get rid of lice, there are a few very important steps you need to take. A breakdown of the different types of otc and prescription medications from the CDC website can be found here:
Prescription and otc lice treatment
- Use a fine-tooth comb after applying medication to hair. This removes the dead lice and eggs. Be sure to put on clean clothing after treatment and wash the dirty clothing. Be sure not to use conditioner before applying the lice medication.
- Do not wash hair for 1-2 days after treatment to assure the lice have been killed
- While treating for lice, wash all bedding and clothing that may have contact with lice. Wash in hottest water possible and dry on high heat.
- Vacuum furniture that may have come in contact with lice. Head lice survive less than 1–2 days if they fall off a person and cannot feed; nits cannot hatch and usually die within a week if they are not kept at the same temperature as that found close to the human scalp.
- Wash combs, brushes, hair clips, etc in hot water for at least 30 minutes to avoid reinfection.
- Depending on the treatment, you may have to retreat 7-9 days after initial treatment to avoid reinfestation.
- Note, some anecdotal treatments, with essential oils and mayonnaise (believed to suffocate the lice) may have some effect on killing the lice, however, it is believed that much of the effectiveness of this method is the use of the fine comb, pulling the lice and eggs out of the hair.
- Do not treat with same medicine more than twice. If the treatment isn’t effective the lice may have built up a resistance to it.
- Keep medicine out of the eyes
- Avoid further skin exposure and able. After using, wash hair in sink, to avoid showering or bathing.
- For more tips on how to mitigate and treat head lice, visit the CDC website.
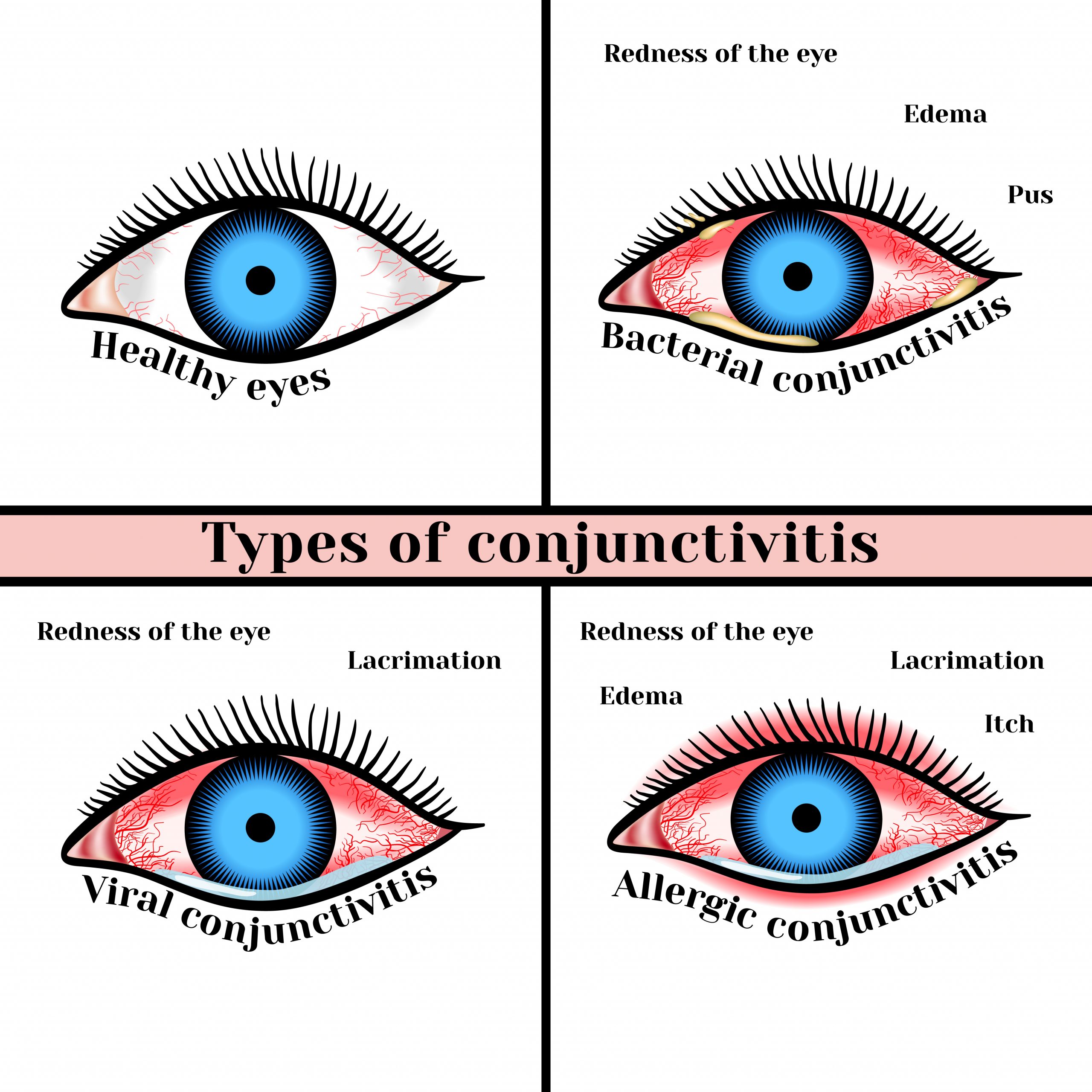
3. Pink eye. AKA Conjuctivitis
This is a condition where the conjunctiva, the thin membrane lining the eyelid and eye, becomes infected or irritated. This in turn can leave the white part of the eye pink or red due to the infection or irritation. Eyes become watery, itchy, and discharge, especially upon awakening can appear.
There are three types of pink eye, viral, bacterial, and allergic. Symptoms and treatment vary depending on type of pinkeye.
Viral conjunctivitis
Viral pink eye is caused by a virus such as a cold or other respiratory virus. It starts in one eye and can easily travel to the other eye, and even to other people as it is highly contagious. Antihistamines, decongestants, and eye drops can help symptoms of this type of pink eye.
It usually resolves within 1-2 weeks without treatment.
Bacterial conjunctivitis
This type of pinkeye is caused by bacteria and is highly contagious, just like viral pink eye. There is more mucus and crusty, greenish-yellow discharge associated with bacterial pink eye. Eyelids can stick together from this discharge upon awakening. This type of pink eye needs to be treated with topical antibiotics or drops. It can cause damage to the eye if not treated.
Allergic conjunctivitis
Symptoms include itchy, puffy, watery eyes. As the name implies, this type of pink eye is caused by allergens, such as pollen, pet dander, and dust mites. This type of conjunctivitis is found in both eyes at the same time, and treatment is symptomatic. Antihistamines and eye drops along with avoiding the allergen if possible are among the most effective treatments. Running a hepa filter in the bedroom can help reduce allergens.
Symptomatic treatments of all forms of pink eye
To relieve the discomfort of pink eye
Green tea and tulsi tea bags, steeped and cooled and placed over the eyes can offer some anti-inflammatory and irritated eyes. Colloidal silver, an antibacterial solution, applied to outside of eyelids when dealing with viral and bacterial forms of pinkeye can help avoid spread of pink eye. Do not replace this with care provided by your primary care provider, however.
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
Cellulitis can be Life Threatening
Drugs That Affect Blood Sugar and Hypoglycemia- A Medical Emergency
Medications can be lifesaving; however, many have unwanted effects. Almost every drug class has medications that can affect blood sugars and even mask high and low glucose levels. From blood pressure meds to inhalers, steroids, antibiotics, antifungals and diuretics,...
Medical Preparedness – Diabetes
Do you have an extra glucometer in your supplies? A chronic condition such as diabetes can be life threatening if our fragile medical supply chain is disrupted and medication or supplies to test are not available. Having adequate supplies- an extra glucometer with...