If you’re considering Jase, chances are you’ve paused and thought, “This makes sense, but I still have a few questions.”You’re not alone. Here are the most common ones we hear, answered plainly. Is this really doctor-prescribed? Yes. Every Jase order is reviewed by a...
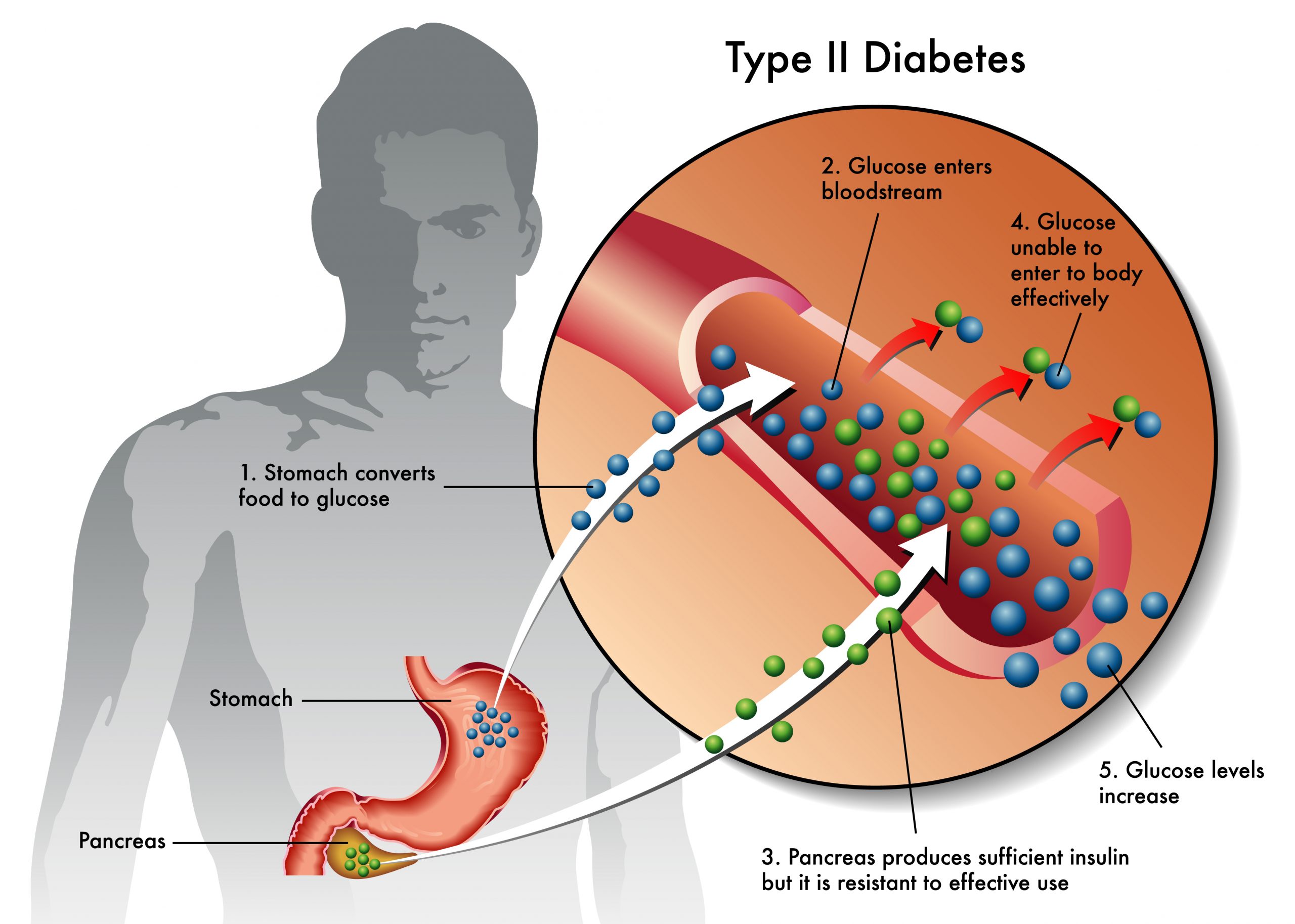
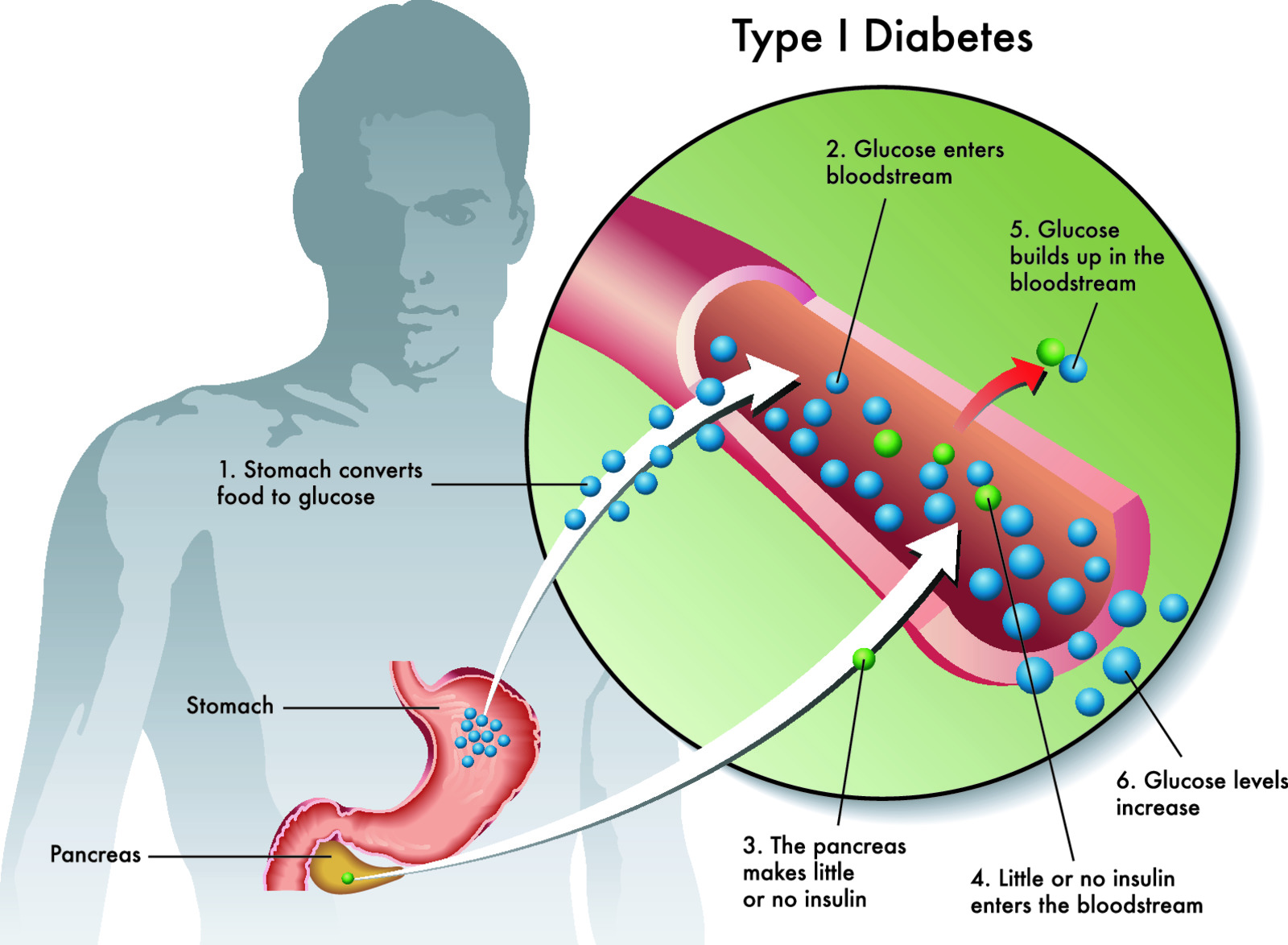
Drugs That Affect Blood Sugar and Hypoglycemia- A Medical Emergency

Medications can be lifesaving; however, many have unwanted effects. Almost every drug class has medications that can affect blood sugars and even mask high and low glucose levels. From blood pressure meds to inhalers, steroids, antibiotics, antifungals and diuretics, the likelihood of you or someone you know using a drug that affects glucose levels. There are too many to list. Below are just a few examples:
A few of the many drugs that increase blood sugar (hyperglycemia): (NIH database)
- Alcohol (decreases blood sugar after several hours of excessive intake)
- Antibiotics (Dapsone, Rifampin)
- Antidepressants (Zyprexa, risperdal, Clozaril, Seroquel, Abilify, Geodon, lithium)
- Beta-2 stimulators (Proventil, Alupent, Serevent, Foradil, Brethine, Theo-Dur)
- Corticosteroids (Prednisone, Decadron, DepoMedrol)
- Dilantin (phenytoin)
- Estrogens (Premarin, hormone replacement therapy)
- Fluconazole
- Heart and blood pressure medications (amiodarone, beta blockers(non insulin dependent diabetics), calcium channel blockers, catapress, diuretics)
- Oral contraceptives (Birth control pills)
- Niacin or nicotinic acid
- Thiazide diuretics
- Thyroid hormones (Synthroid, Levothroid)
If on a continuous glucose monitor acetaminophen (Tylenol) interferes with sensors resulting in a false low glucose reading and should be avoided.
A few of the drugs that decrease blood sugar (hypoglycemia): (NIH database)
- Alcohol (acute excess amounts)
- Aspirin and other salicylates in larger doses
- Cibenzoline and quinidine (heart arrhythmia drugs)
- Indomethacin (Indocin)
- Levofloxacin
- Trimethoprim-sulfamethoxazole
- Metformin when used with sulfonylureas
- Heart and blood pressure medications (ACE inhibitors, beta blockers, Norpace, Quinidine)
One common drug that masks low blood sugar
If diabetic (especially insulin dependent) and taking beta blockers the symptoms of low blood sugar may not be apparent. Beta blockers block the effects of norepinephrine. Norepinephrine, along with epinephrine are released into the bloodstream during hypoglycemic episode. In turn the release of these hormones causes the early symptoms of hypoglycemia such as tremor, sweating, rapid heartbeat, and anxiety. If diabetic and taking beta blockers monitor glucose levels closely even when you don’t have signs of low blood sugar.
Signs of low blood sugar (below 70 mg/dL or less)
Low blood sugar, especially in a diabetic, can be more dangerous and even a medical emergency if not treated in time.
Common signs of low blood sugar are:
- Fast heartbeat
- Shaking
- Sweating
- Nervousness or anxiety
- Irritability, anger or confusion
- Dizziness
- Hunger
During sleep, low blood sugar symptoms may include sweaty sheets and sometimes nightmares
Signs of severe low blood sugar (below 54 mg/dL or by symptoms listed below)- Medical emergency
- Loss of coordination
- Difficulty speaking or slurred speech
- Blurry or tunnel vision
- Inability to eat or drink
- Muscle weakness
- Drowsiness
If left untreated hypoglycemia can result in coma, seizures and in rare cases, death
Causes of Low Blood Sugar
There are many reasons why for low blood sugar, including:
- Taking too much insulin and/or not taking it on time
- Not eating enough carbs after taking insulin
- Poor diet- not eating a balanced protein, carbs and fat diet
- The amount and timing of physical activity.
- Drinking alcohol.
- Hot and humid weather.
- Unexpected changes in your schedule.
- Spending time at a high altitude.
- Going through puberty
- Menstruation
- On medication that causes low blood sugar
- Severe liver or kidney disease
- Severe infection
- Advanced heart disease
- Pancreatic or adrenal tumors
- Drinking alcohol at night
What to do if you or someone you know has low blood sugar. The CDC website has tips on managing and treating hypoglycemia:
For low blood sugar between 55-69 mg/dL, raise it by following the 15-15 rule:
Have 15 grams of carbs and check your blood sugar after 15 minutes. If it’s still below your target range, have another serving. Repeat these steps until it’s in your target range. Once it’s in range, eat a nutritious meal or snack to ensure it doesn’t get too low again.
These items have about 15 grams of carbs:
- 4 ounces (½ cup) of juice or regular soda.
- 1 tablespoon of sugar, honey, or syrup.
- Hard candies, jellybeans, or gumdrops (see food label for how much to eat).
- 3-4 glucose tablets (follow instructions).
- 1 dose of glucose gel (usually 1 tube; follow instructions).
Tips to keep in mind:
- It takes time for blood sugar to rise after eating. Give some time for treatment to work. Following the 15-15 rule helps.
- Young children usually need less than 15 grams of carbs, especially infants and toddlers. Ask your doctor how much your child needs.
- You should avoid eating a carbohydrate with lots of fiber, such as beans or lentils, or a carb that also has fat, such as chocolate. Fiber and fat slow down how fast you absorb sugar.
- Check your blood sugar often when lows are more likely, such as when the weather is hot or when you travel.
Treating Severely Low Blood Sugar- (below 55mg/dL)
Not treatable by 15-15-15 rule
Make sure your family members, friends, and caregivers know your signs of low blood sugar so they can help treat it if needed.
You also may not be able to check your own blood sugar or treat it by yourself, depending on your symptoms.
Injectable glucagon is the best way to treat severely low blood sugar. A glucagon kit is available by prescription. Speak with your doctor to see if you should have a kit. Be sure to learn how and when to use it. Let family members and others close to you know where you keep the glucagon kit and make sure they’ve been trained in how to use it too.
It’s important to contact a doctor for emergency medical treatment immediately after receiving a glucagon injection. If a person faints (passes out) due to severely low blood sugar, they’ll usually wake up within 15 minutes after a glucagon injection. If they don’t wake up within 15 minutes after the injection, they should receive one more dose.
When the person is awake and able to swallow:
- Feed the person a fast-acting source of sugar (regular soft drink or fruit juice).
- Then, have them eat a long-acting source of sugar (crackers and cheese or a sandwich with meat).
- It’s also important that friends, family, co-workers, teachers, coaches, and other people you may be around often know how to test your blood sugar and treat severely low blood sugar before it happens.
A medical ID, usually a bracelet or necklace, can be critical in keeping you safe and healthy. Emergency medical technicians are trained to look for a medical ID when caring for someone who can’t speak for themselves.

When To Call 911
If any of the following happens, your friend, relative, or helper should call 911:
- You pass out and no glucagon is available.
- You need a second dose of glucagon.
- You had glucagon but are still confused.
- Your blood sugar stays too low 20 minutes after treatment or doesn’t respond to your usual treatments.
- Or call 911 anytime you are concerned about your severely low blood sugar.
After You Have Low Blood Sugar
If your low blood sugar was mild (between 55-69 mg/dL), you can return to your normal activities once your blood sugar is back in its target range.
After you have low blood sugar, your early symptoms for low blood sugar are less noticeable for 48 to 72 hours. Be sure to check your blood sugar more often to keep it from getting too low again, especially before eating, physical activity, or driving a car.
If you used glucagon because of a severe low (54 mg/dL or below), immediately call your doctor for emergency medical treatment. If you have had lows several times close together (even if they’re not severe), you should also tell you doctor. They may want to change your diabetes plan.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
FAQ: Our most commonly asked questions about Jase
Medical Readiness: What Really Kills First
When Disaster Strikes, It’s Not Hunger or Thirst That Takes the First Lives In every disaster zone, from hurricanes in the Caribbean to war zones in Ukraine, the pattern is the same. People worry about food and water, but it’s infection that kills first. A small wound...
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole *Disclaimer: This article is for educational purposes and does not constitute medical advice. Always seek professional guidance.* In the evolving...