If you’re considering Jase, chances are you’ve paused and thought, “This makes sense, but I still have a few questions.”You’re not alone. Here are the most common ones we hear, answered plainly. Is this really doctor-prescribed? Yes. Every Jase order is reviewed by a...
Staying Safe in the Summer Heat: Tips to Beat the Heat and Avoid Heat-Related Illnesses

Summer- a time of long, endless days of warm weather that children across the country look forward to when school lets out. Swimming, hiking, bicycling, and even setting up camp and stargazing in the backyard are the stuff that fond memories are made of.
All these fun activities, however, can pose potential illness or danger, especially when its hot outside.

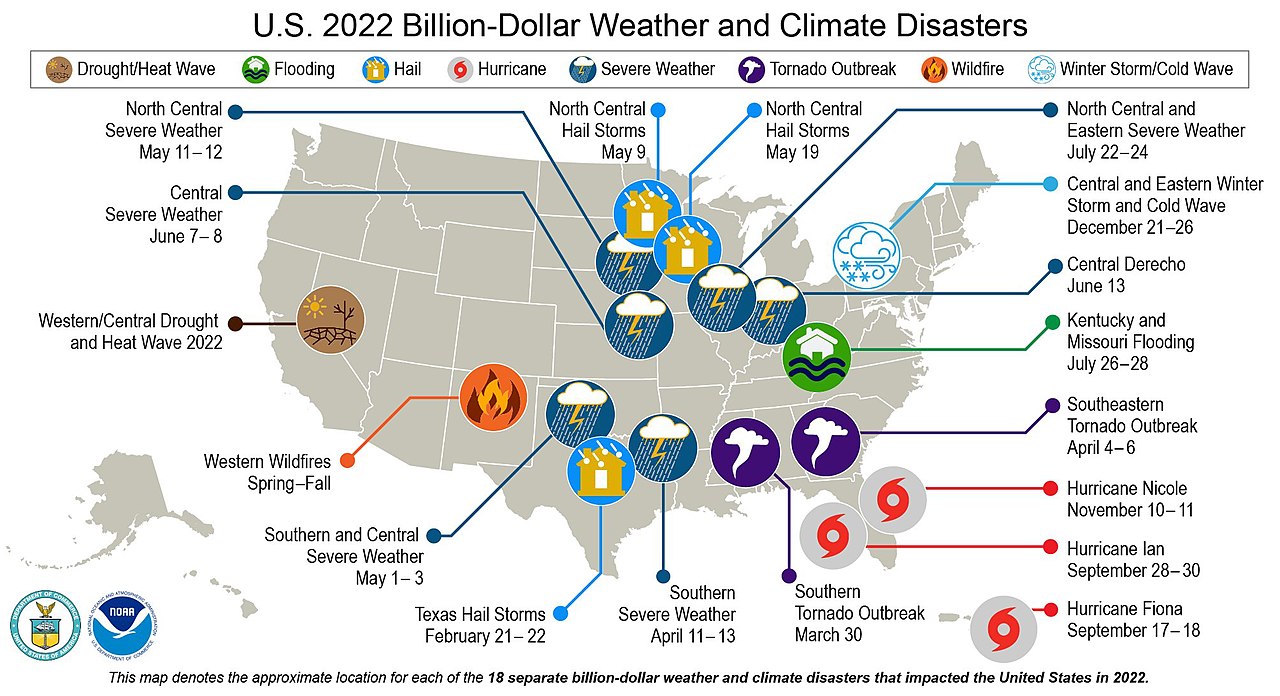
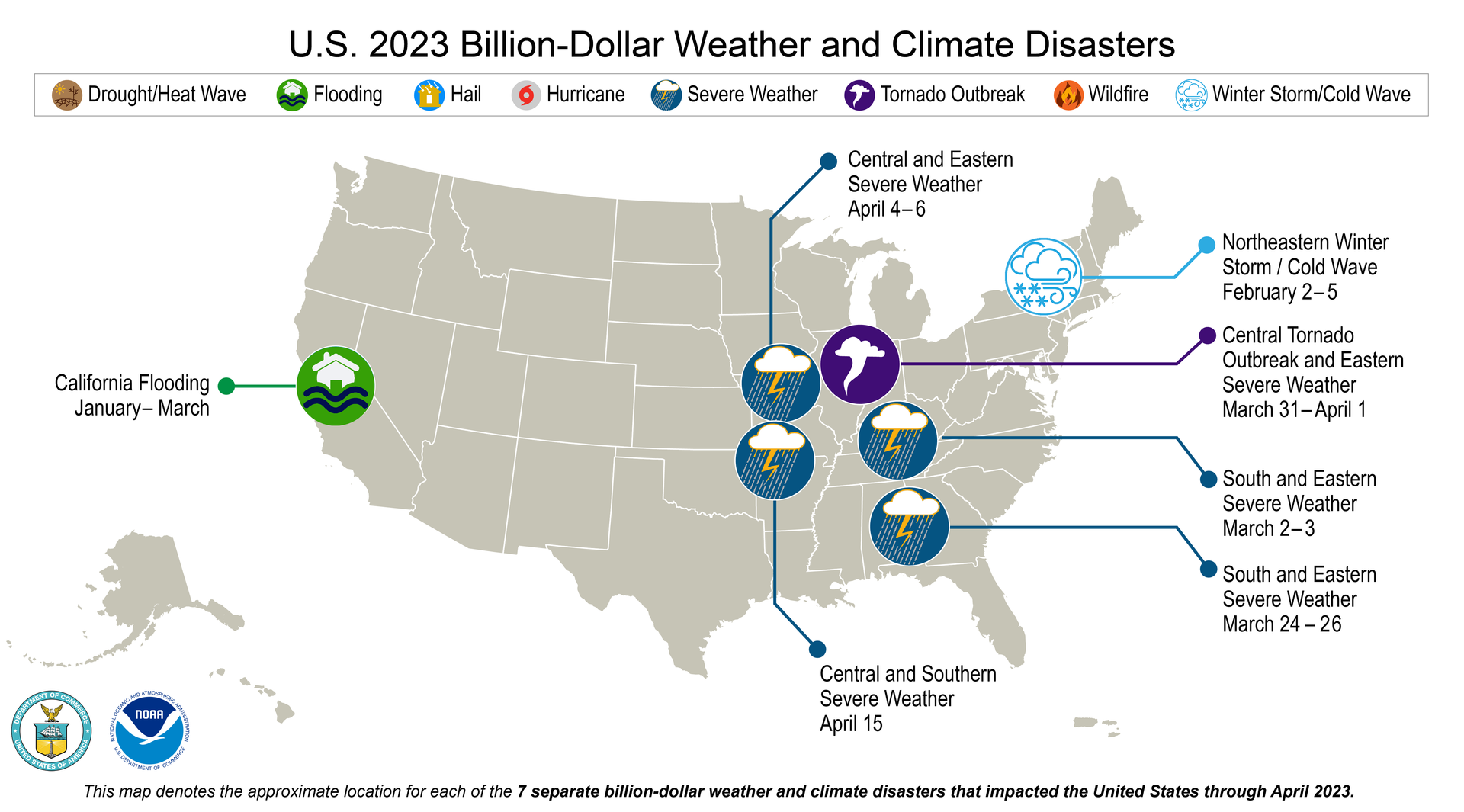
Heat wave sweeps the country
Record breaking heat was recorded in Miami, Austin and Phoenix over the past few days. Even Portland Oregon, usually known for its cooler weather broke daily records. You don’t have to have record breaking weather to suffer overexposure to sun and heat. One recent and very heartbreaking story out of Vancouver was of a one-year-old child that died from heat stroke in a car while the outdoor temperature was only 70-75 degrees. The inside of the car reached 110 degrees. According to the National Safety Council on average more than 38 children from the ages of 1-15 die from heatstroke, mostly from being in a hot car. July is the month that most of these deaths occur, according to the website.
That quick trip into the store for a quart of milk could prove dangerous, even fatal to a young child left unattended in a vehicle.
Populations most at risk for heat related illnesses
Heat related illnesses can affect anyone but certain populations are more prone than others. These include:
Age: Infants, young children, and elderly individuals are more susceptible to heat related illnesses. Both children and elderly have a reduced ability to regulate body temperature.
High heat exposure: High temperatures for extended periods, especially during a heat wave, can put anyone at risk for heat related illness.
High humidity: When the humidity is high, the body’s ability to cool down through sweating is reduced, increasing the risk of heat-related illnesses, including heat stroke.
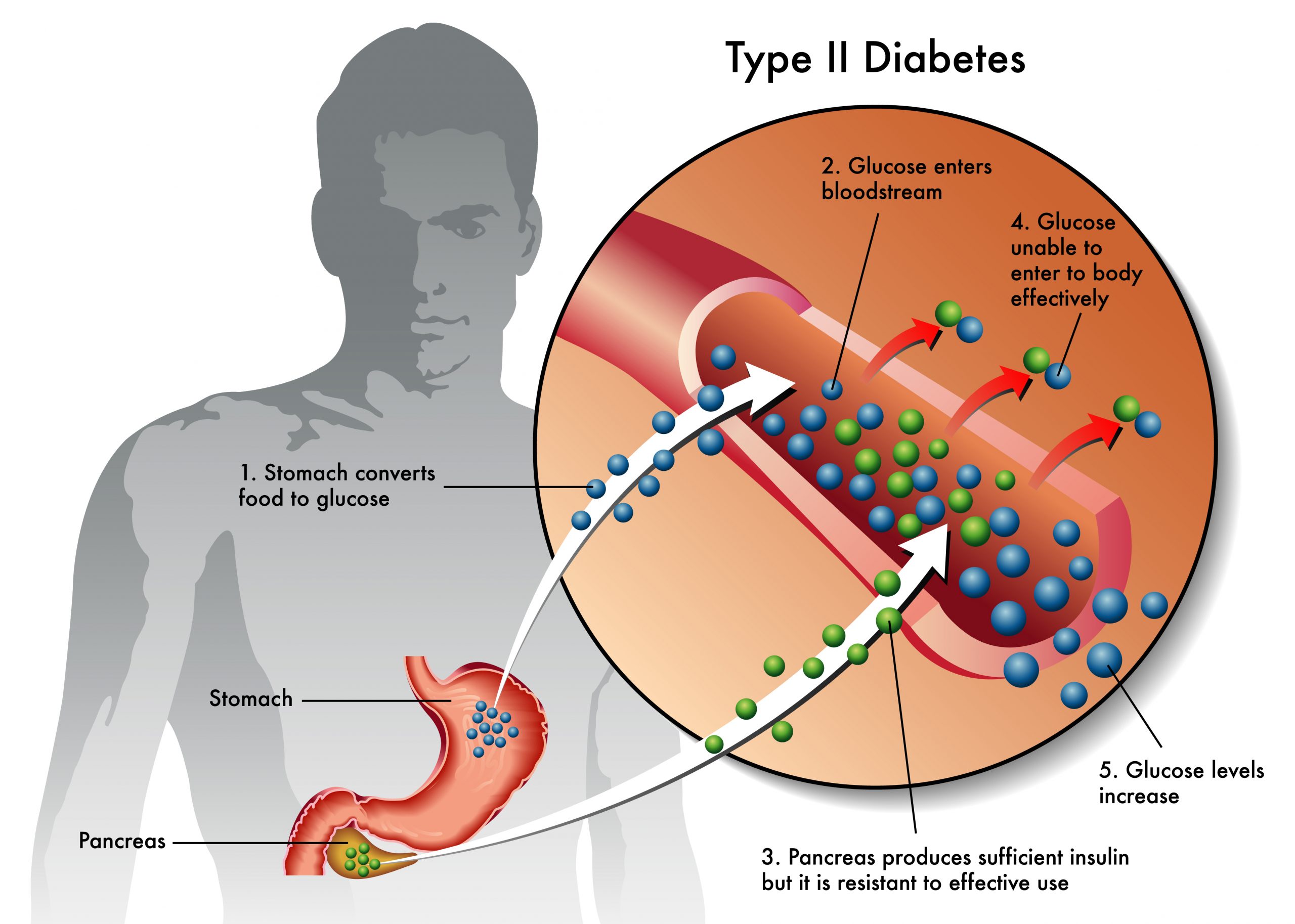
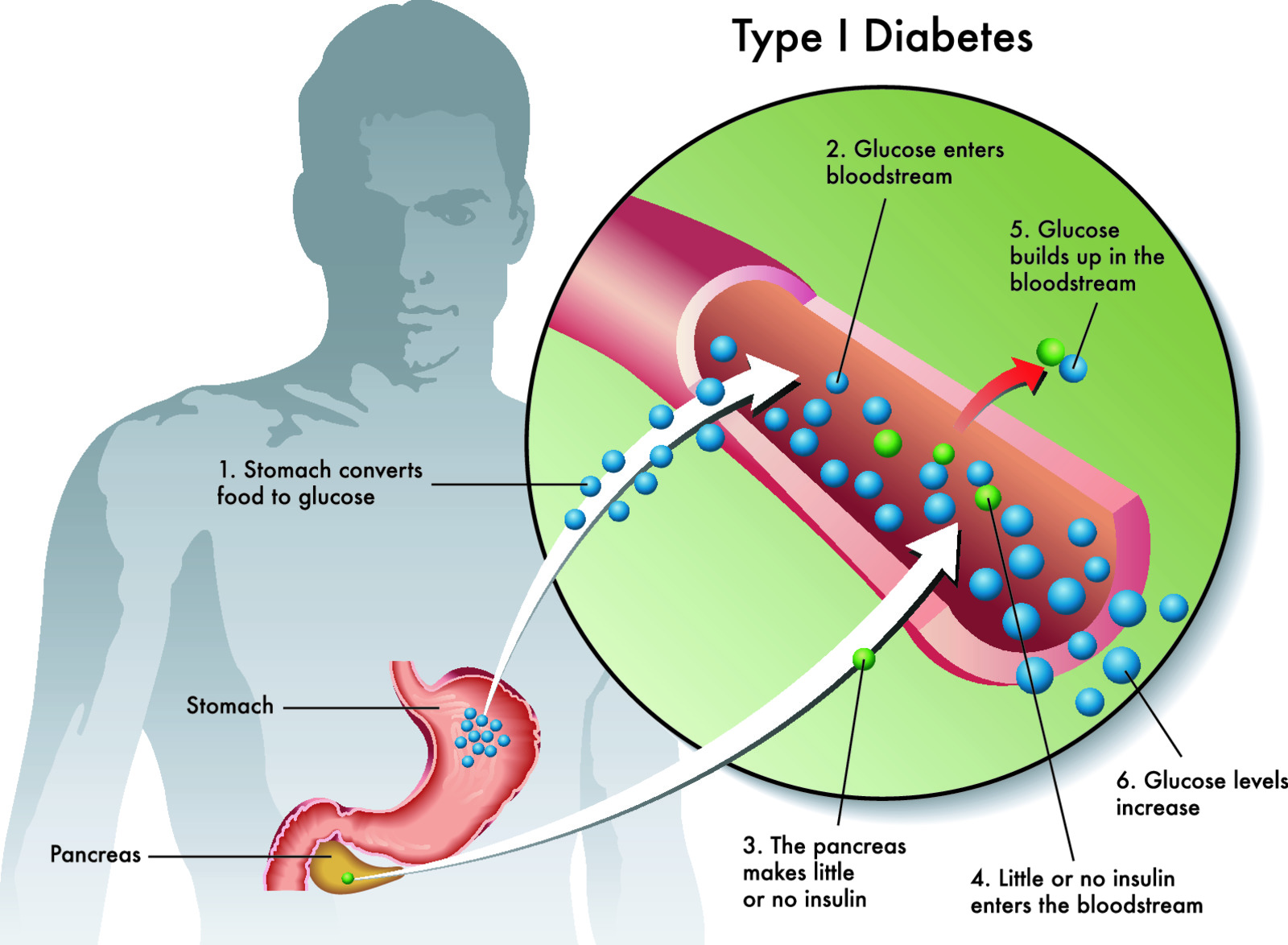
Chronic health conditions: Certain medical conditions, such as heart disease, lung disease, obesity, and diabetes, can reduce the body’s ability to handle heat stress, making individuals more susceptible to heat stroke.
Medications: Some medications can interfere with the body’s ability to regulate temperature, leading to heat exhaustion or heat stroke. Take precautions if on any medications. The following is a brief list- check your specific medication for more information:
Anticholinergic drugs: These medications block the action of acetylcholine, a neurotransmitter that plays a role in various bodily functions, including sweating. By reducing sweating, these drugs can hinder the body’s ability to cool down effectively. Examples include certain antihistamines, tricyclic antidepressants, and medications for overactive bladder.
Diuretics: Diuretics, commonly known as water pills, increase urine production, which can lead to dehydration. Dehydration impairs the body’s ability to regulate temperature, making it harder to dissipate heat. Some diuretics cause electrolyte imbalances which can further compromise health.
Beta-blockers: Beta-blockers are used to treat various conditions, including high blood pressure and heart conditions. They can reduce the heart rate and limit the body’s response to heat, potentially interfering with temperature regulation.
Psychotropic medications: Certain medications used to treat mental health conditions, such as antipsychotics and mood stabilizers, can affect the body’s heat regulation mechanisms, leading to increased heat sensitivity. This is an often-overlooked class of drugs. Be sure to check with pharmacist or read side effects of these drugs before heading off into the heat.
Antidepressants: Some antidepressants, especially those that affect serotonin levels, can impact the body’s thermoregulatory systems, potentially causing an increased risk of heat-related issues.
Antihypertensive medications: Some medications used to lower blood pressure, such as alpha-blockers, can impact the body’s response to heat and affect blood flow to the skin.
Alcohol and drug use: Alcohol and certain drugs can impair the body’s ability to regulate temperature and increase the risk of heat stroke.
Physical activity: Physical activity, particularly in hot and humid conditions, can raise the risk of heat stroke, especially if adequate hydration is not maintained. If not acclimated to the heat this can pose a serious health risk.
Lack of acclimatization: Individuals who are not accustomed to hot weather or are not acclimatized to the heat may be more susceptible to heat stroke. This is especially true for those living in or working in air-conditioned buildings.
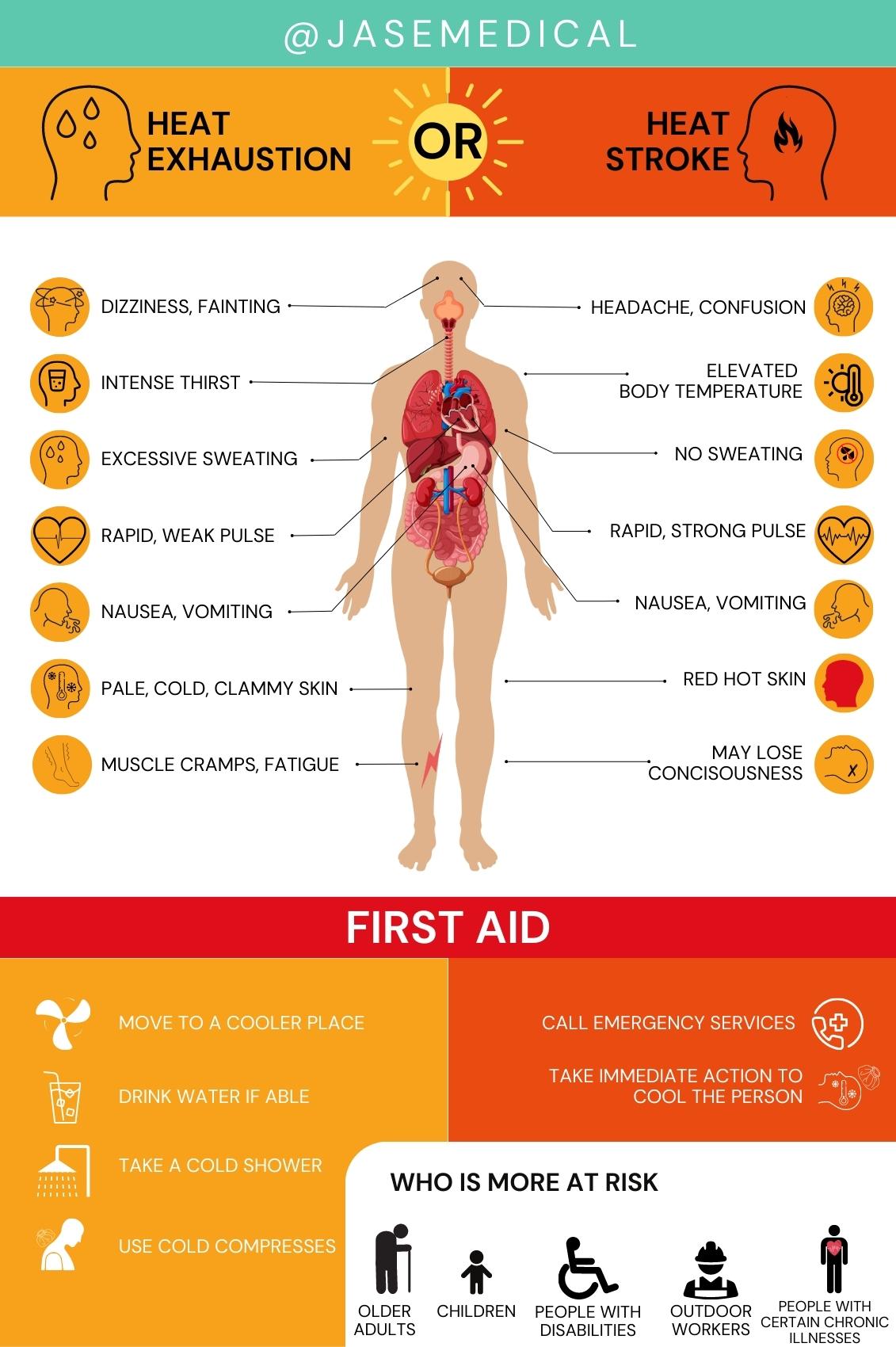
Heat exhaustion and heat stroke- know the signs and what to do
Heat exhaustion and heat stroke are two distinct heat-related illnesses, with heat stroke being the more severe condition.
CDC excerpt on heat exhaustion and heat stroke:
Avoid
When the temperature is very high stay indoors. If you must go outside, dress properly and take breaks often. Know who is at high risk for heat stroke and heat exhaustion.
Tips to Beat the Heat
- Drink plenty of water! (I will add that electrolyte drinks such as these can replace lost fluids and prevent electrolyte imbalance
- Check on friends and neighbors at high risk for heat-related illness
- Find airconditioned places to cool off (shopping malls and libraries)
- NEVER leave kids or pets in a closed, parked vehicle
- If you go outside, remember:
- A hat
- Sunscreen (spf 15 or higher)
- Lightweight, light-colored, loose-fitting clothing
- Water
- Limit time outdoors. Take breaks often
- Know who is at high risk:
- Infants
- Young children
- Older adults
- People with chronic medical conditions
Spot
Know the signs of heat stroke and heat exhaustion.
Heat Stroke
Signs & Symptoms
- Very high body temperature (above 103°F)
- Red, hot, and dry skin (no sweating)
- Rapid, strong pulse
- Throbbing headache
- Dizziness
- Upset stomach
- Confusion
- Passing out
Heat Exhaustion
Signs & Symptoms
- Heavy sweating
- Paleness
- Muscle cramps
- Tiredness
- Weakness
- Dizziness
- Headache
- Upset stomach or vomiting
- Fainting
If you see any of these signs, get medical help immediately.
Treat
While waiting for medical attention, you can help someone with heat stroke or heat exhaustion.
Heat Stroke
Move the victim to a shady area or indoors. Do not give the person fluids.
Cool the body by:
- Placing person in a cool (not cold) bath or shower
- Spraying with a garden hose
- Sponging with cool water
- Fanning
Continue efforts to cool the person until help arrives or his or her body temperature falls below 102°F and stays there.
Heat Exhaustion
Get medical attention if symptoms get worse or last longer than one hour.
Cool the body with:
- Cool, nonalcoholic beverages
- Rest
- A cool (not cold) bath, shower, or sponge bath
- Moving to an airconditioned room
- Wearing lightweight clothing
Seek medical help immediately if symptoms are severe or if victim has heat problems or high blood pressure.
Taking just a few precautions will ensure you and your child will have a fun and adventure filled summer.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
FAQ: Our most commonly asked questions about Jase
Medical Readiness: What Really Kills First
When Disaster Strikes, It’s Not Hunger or Thirst That Takes the First Lives In every disaster zone, from hurricanes in the Caribbean to war zones in Ukraine, the pattern is the same. People worry about food and water, but it’s infection that kills first. A small wound...
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole *Disclaimer: This article is for educational purposes and does not constitute medical advice. Always seek professional guidance.* In the evolving...