Part 3 of 5
“Why are you back home?” your wife asks, after hanging up the phone from her conversation with the pediatrician. “Did you forget something?”
You briefly relay what transpired. The sign on the office door that read “closed”, the strange radio announcements about staying home, a possible bioterror attack not too far from your home. Your wife turns on the tv. Every station is carrying the same news. From what you can tell the “early flu” you read about while on vacation turned out to be some sort of bioterror attack.
Your two boys were headed to school at this very moment. You call the younger on their cellphone since the older boy was driving. “Come home immediately” you order After explaining the situation the boys head back home. “Don’t go anywhere, don’t stop to pick anything up at the store, come straight home.” You tell them.
You sit down, your head is reeling. You think to yourself “What should I do? Or not do?”
First things first. You check on your daughter. She seems to be comfortable. She is holding down fluids and is listening to music in her room. Hopefully she doesn’t get any worse, so you won’t have to take her to the clinic. You wonder out loud if the clinics are even open during this crisis and make a mental note to call your family doctor’s office later that day.
The boys just arrived from their trek to school and back. Apparently, their phones had texts telling them to go home and stay home. They thought it was a prank. Their first impression was a hacker had been able to access the school records and sent out a phony alarm.

More news is pouring in from the television. Apparently, the attack was carried through the mail system. This was vaguely reminiscent of the post 911 Anthrax attacks. Back then, the mail was addressed to certain politicians and media outlets. The Anthrax was found in letters, when upon opening the spores were released, killing 5 people, and injuring 17 others.
As usual, the news outlets were tight lipped about what was going on. From what you can surmise the attack seemed random and the bioterror agent causes early flu like symptoms. Apparently, the agent was/is being distributed in “free” samples of organic lavender scented body powder. The clinics and hospitals had been diagnosing this as early season influenza based on symptoms alone until one clinician decided to have a lab specimen tested.
Since the attacks had been considered random and labeled bioterror the whole country had been placed in a type of “lockdown”. You wonder if the bioterror agent is contagious, if your family has received any of these organic powder samples, if so, have they opened them, was anyone other than your daughter sick. Thankfully all the answers were a resounding NO.
Reports were flowing in from all parts of the nation. Even Alaska was affected. No mention of Hawaii. People were advised to stay home, wait further instruction and phone their health care provider if they had opened any sample packages labeled organic powder. Anyone with flu like symptoms was also to contact their primary care providers. An advisory to not open mail was issued.
You ask your wife and children if they had gotten the mail from the post office since getting back from the cabin. No one had. You breathe a sigh of relief.
“Do you have any clue what is going on?” you ask your paramedic neighbor. “At this point we are to wear our hazmat suits and be fully prepared and equipped for any respiratory agent exposure”’ he said. I am guessing we will know more soon. I sure hope I don’t get called out on a call from whatever this attack is. People are already starting to panic and are calling 911 for almost anything.”
You hang up the phone. Reports on local news outlets are of people panic buying at the stores, even though they were told to stay home. The grocery stores were unable to handle the overbearing crowds, pushing their way through the stores. Panic buying on bottled water and junk food seemed to fly off the shelves according to news outlets, and videos of people pushing carts full of potato chips, beer, bottled water, and soda pop.
Hospitals were also getting hit hard. Mass hysteria had hit. People were pouring into the Emergency rooms with anxiety, shortness of breath and vague symptoms of not feeling well. It was exactly what the authorities were trying to keep from happening by ordering everyone to stay home until they could figure out what was going on.
You decide the last thing anyone needed to do was to be out in that mob. You and your wife decide to take stock of what you have in the house to survive the next week. Since you had returned from your vacation you had a lot of leftover food. Canned food, fresh fruit, bottled water, etc. Plenty of first aid supplies, along with ample over the counter pain relivers, etc. There was no reason to leave home as long as your daughter continued to recover from her diarrhea.
The news reports continued well into the night. In the distance you hear sirens racing down the highway. Many more than usual. You sit back in your favorite recliner. Exhausted from your trip and now the news, you fall into a fit full slumber.
As the sun breaks the horizon you become aware the tv had been on all night. One of your sons had been up watching it the entire time. “Any new developments?” you ask. “Tularemia or something like that, “he said. “It’s what the terrorists put in the powder samples in the mail.” “Never heard of it” you said. “Did you look it up?” “I did”, he said. “Seems there are different types. The one the terrorists used are airborne. It is a bacteria that takes only a few to infect someone. One good thing is that you can’t catch it from someone who has it. But it can be fatal if not treated. Guess since this is a random attack the government decided to just stop mail delivery and have everyone stay home until they could figure out what to do.”
How do you spell that? Did they say what the treatment is? You ask. Your son spells out Tularemia. “Treatment is antibiotics”. Guess the government has a large supply of antibiotics for such an attack but since this is such a random event, they aren’t sure they have enough, or where in the States the antibiotics should go to.” You ask if he knows what antibiotics were effective against Tularemia. He didn’t know. You recall your Jase case and the small emergency antibiotic guidebook that came with it. Ciprofloxacin and Doxycycline are both mentioned in the booklet as effective against Tularemia. The Jase Case includes both antibiotics. You breathe a sigh of relief. You sincerely hope you don’t have to use these, but if you do, you and your family have your own emergency supply.
Part 2 of 5
Your days at the cabin blissfully melt together, the mornings filled with a steamy hot mug of coffee, fresh eggs from the local farm cooked on the woodstove and anticipation of what the day’s activities will bring. The air is crisp and clean. There is a bit of a chill in the air. “Fall seems to be coming early this year,” you note. Each day is an adventure. Earlier in the week your wife had taken a walk down along the river which feeds the pond. She had been eyeing the blackberry patches growing along the river’s edge. Each day she reported on how ripe the berries were. “Today is berry picking day” she declared.
Trying to find a way to get out of her idea of fun and yours of work, you offer to head down the hill and pick up some ice cream to accompany the berries. The boys can help her pick and cut back the theory stems while she picks. Your daughter also wants to go to town. Her stomach has been acting up a bit and she wants to pick up something to calm it.
Your trip down the hill and back was uneventful. You pick up a local newspaper while in town.
Later that evening after ice cream and berries, you settle in to read the newspaper. The usual headlines-a trucker’s strike, upcoming elections, the flu season is early this year, etc. You think to yourself that you haven’t missed much and throw the paper into the fire starter box.
The next morning you are awoken by your wife who tells you your daughter has been having diarrhea all night. She hasn’t been feeling well for the past day, having stomach cramps and nausea. She believes she just ate something that didn’t agree with her. The Pepto Bismol seems to help with the nausea but not much with the diarrhea. At this point she isn’t showing any signs of dehydration.

Your sons were fine, they were ready for a day of collecting wood and cooking hotdogs over an open fire for lunch. 2 more days and you will be back in “civilization” you muse. A day to unpack and then back to work. The vacation has been refreshing, but you are looking forward to sleeping in your own bed and enjoying the modern conveniences of life, such as your electric stove and heater. One thing you are contemplating, is how much your family depends on the system. From heating and cooking (both electric) to medicines and your food supply. The newspaper mentioned a trucker’s strike. If the trucks all stopped running, what would happen? How would food get delivered? How about the parts for their cars? How about, heaven forbid, medical supplies and medicine? He knew very little about trucking logistics, or food logistics for that matter. His specialty was engineering.
All of a sudden, you feel very vulnerable. You had purchased your Jase cases for the family after talking to your neighbor, a paramedic. He seemed to be aware of the supply chain and how fragile it was. “You recall the conversation you had with him that convinced you that at the very least antibiotics should be a priority in case of an emergency or supply chain disruption. You had discussed this with your wife, who was in full agreement.
Looking back on this decision you are grateful you took the plunge and purchased the cases. It saved your vacation-not having to run to the clinic and disrupt the family vacation. Your thumb was healing nicely, and you only have a few days left of antibiotics to finish the course.

You decide that when you get back home you should assess what else is lacking in your family’s preparedness. The next 2 days flew by, and you were back home. Your yard looked a little unkempt. The grass and weeds were starting to take over. “I wonder if the HOA would allow some neatly kept planter boxes in place of the grass. We could grow some tomatoes, lettuce, squash. After the boxes were installed the upkeep and water bill would be lower. You relish the idea of fresh vegetables with less yardwork, lower water bill(set boxes up on timer) and lower grocery bills.
Your daughter is especially happy to be home, with modern plumbing and her cozy bed. Her diarrhea had not slowed down. Your wife notes she seemed to be getting a little dehydrated and that your daughter’s stool was very foul smelling. The first aid bag contains oral rehydration powder, which you mix with water and give to her. Your wife calls your daughters pediatrician. She says to just continue to offer your daughter the rehydration solution, bland foods and monitor for now. She states that most cases of diarrhea clear up on their own after a week or so. You take mental note that it has been 5 days since your daughter started feeling ill.

Monday morning seemed to come too fast. You are refreshed from your vacation and eager to show coworkers the cabin and wildlife pictures you took on your phone. As you drive into the parking lot you notice a sign on the front door. “Closed until further notice it reads.” Your phone had been on airplane since last night. You take your phone off airplane and a series of texts start pouring in. “Bioterror attack – stay home, office closed until further notice. You have missed 2 voicemails and 6 phone calls starting Sunday afternoon. It hadn’t occurred to you to turn on the radio on your way to work. You and your family had been offline since yesterday, even your children agreed it was nice to get away from all the electronics. You all agreed to catch up on news etc. for the afternoon, then take a break from the internet and media until Monday.
Heading home, you realize that there weren’t many people on the road. The streets seemed eerily quiet. Even the grocery stores were closed. “What in the world is going on?” you wonder. You turn on the radio. “Mysterious illness…. Believed to be bioterror attack…. If you live in the vicinity of…….Stay home……” You rush home to find your wife on the phone with the pediatrician. Your daughter isn’t doing very well. Her diarrhea hasn’t let up and she is getting more dehydrated, even when given the rehydration solution. Her pediatrician is quizzing your wife on what your daughter had eaten and her activities. When your wife relayed her daughter had been swimming in the pond while on vacation her pediatrician suggested she may have become infected with an intestinal parasite, Giardia. Giardia, she states, is very common, and can be found in contaminated waters, lakes, food, daycare settings, etc. It is transmitted via oral to fecal route. Her pediatrician recommends starting your daughter on an oral antibiotic. She offers to call in a prescription, however it may not be available, given the unknown nature of the bioterror attack. You pull out your daughters Jase case, and hand it to your wife. She tells the pediatrician about Jase and reads the 5 antibiotics in the case. “Will any of these work?” your wife asks. The pediatrician instructs your wife to give your daughter metronidazole, one of the antibiotics in the Jase Case. She further instructs her on disinfecting surfaces with 1 cup bleach to 1 gallon water to kill the parasite, monitor your daughter and call her if there isn’t improvement in the next few days. Your wife thanks the doctor and hangs up the phone.
You are slowly realizing that the world as you had known it has changed.
Part 1 of 5
Medical care not available. What to do?
You have decided to load the family up in the car and take off deep into the mountains to your friends off grid cabin to get away and regroup from this crazy world. You planned for a full week of fishing, hiking, reading, and eating too much. Your fishing pole and tackle box are tucked safely in the trunk, ready to use as soon as you get to your mountain destination. The car is jam packed with food, water, camping chairs, sleeping bags, camp stove, first aid gear and all the basic amenities to make this a fun and restful trip for all.

The 5-hour trip was uneventful. You stopped at the diner at the base of the mountain for a quick bite of lunch before heading up the hill. The fragrant scent of pine trees, cool fresh air adds to the excitement and anticipation of the well-deserved and needed getaway. Snow was still clinging to various knolls and shaded valleys; winter was not giving in so easy. Overall, the clear skies dotted with fluffy white clouds and plenty of sunshine promised this was going to be a great week.
After several wrong turns (GPS turned out to be unreliable in the mountains) you finally pull out your friends’ directions you had downloaded from the internet and a paper map. You arrive at your destination well before sunset, unpack and head down to the small pond at the bottom of the property. You aren’t alone, the dog and your daughter join you. The pond isn’t too far from the cabin. You can see it from your fishing hole. You hear a pounding of feet behind you coming from the cabin. Before you know it your daughter and dog jump off the dock and into to the water with a resounding splash. “I’m trying to fish,’ you yell, annoyed. “Why don’t you swim on the other side?” Your daughter and dog take off across the pond, racing each other to the other edge of the pond. The water is crystal clear and calm. Once things had settled down and the water was calm you put a squirmy worm on your hook, attach a bobber and weight and cast your line. You settle back and start to relax. This was a good decision “you muse, no tv, no internet, only our family and nature.” In the distance you can see your daughter and dog climbing out of the pond and racing back to the cabin. A few moments later you see your bobber go under. And again, it submerges. You wait patiently while your fish takes the bait, swallowing the hook and worm. Reeling in your catch you see it is a nice size rainbow trout. Holding it firmly with one hand, you use the pliers to extract the hook. “He really swallowed that worm” you noticed. You run the stringer through the gills and mouth and toss it in the water anchoring it to the side of the bank to keep it fresh. As you put another worm on your hook you notice you had scraped your thumb and a line of blood was dripping from the tip. The hook had cut a fine line in your thumb. You hadn’t noticed with all the excitement. Wiping the blood off on a rag, you cast your line in. After an hour of fishing, you bring in 3 more good sized trout, enough to feed the family. Satisfied with your labors you clean your fish and bring them back to the cabin. Your evening was filled with board games, by a crackling woodstove and a large mug of steaming cocoa. A feeling of contentedness swept over you as you fell into a blissful sleep.

Arising the next morning you collect kindling and start the woodstove. The cabin heats up quickly, given the late summer season. Your thumb is feeling achy, and a bit warm. You brush off the pain and cover it with a bandage. You review today’s itinerary. The cabin sits on a 35-mile trail which is in the national forest. According to the map and guides the trails are clearly marked and rated as easy to moderate. Given his children’s ages (daughter 11 and sons, 14 and 16) a 6-mile loop hike would be a good distance to hike.
Armed with binoculars, cellphones (for picture taking) hats, maps, snacks, water, and sturdy shoes you and your tribe take off for the 6-mile loop. Your thumb is still achy and is throbbing and getting red and swollen. Not wanting to interrupt this special family outing you ignore the signs of infection. The hike was a success. You pride yourself on remembering the binoculars, your son was able to spot a bald eagle sitting high above on its perch. The hats also came in handy, as much of the hike was in the midday sun.
Arriving back at the cabin, you can’t ignore your very sore thumb. You soaked it in Epsom salts, but the fiery red thumb was getting more swollen and purulent drainage from the wound started appearing. Suspecting it may be infected you retrieve your first aid kit, which includes your Jase Case You feel fortunate you had thought of obtaining a Jase case for each member of the family, which you keep with your first aid kit. Suspecting an infected thumb, you locate the ordering physicians’ number and call. You describe the injury sustained to your thumb and the symptoms that led you to call.
Given your physicians knowledge of your health history and allergies he advises you start the doxycycline included in your Jase Case. He further advises you review the precautions (can cause sun sensitivity, etc.) and how to take your medication. He also encourages you to call if after 2 days your thumb isn’t doing much better after starting the antibiotic, or if you notice a worsening of symptoms (fever, sweats, worsening drainage, red lines from wound traveling up arm, etc.)
You thank him, relieved you avoided interrupting your family’s vacation with a trip to the local walk-in clinic.

As 2022 marches on, our world is becoming increasing unstable. Worldwide conflicts are causing worldwide, nationwide, and local problems.
We are now faced with out-of-control gas prices, which will have a trickle-down effect, not just at the gas pump, but in every part of our economy and lives. Trucks may soon not find it profitable to deliver food, materials, and even medical supplies. Store shelves, which are already showing signs of shortages and escalating food prices may soon be at a point where the food may be in stock but unaffordable.
Inflation just hit a 4 decade high and there is no end in sight.
 Add to this state and federal agencies warn healthcare providers of imminent cyberattacks.
Add to this state and federal agencies warn healthcare providers of imminent cyberattacks.
“The Cybersecurity and Infrastructure Security Agency (CISA), the Federal Bureau of Investigation (FBI), and the Department of Health and Human Services (HHS). Issued an advisory that cybercriminals were planning on targeting healthcare systems with ransomware for financial gain.”
As I have pointed out in previous articles China and India play an integral part in our medication production and raw materials to make medications. With world events affecting these supply chains we really could be looking at a catastrophe in the making.
Cognitive dissonance-the mental conflict that occurs when beliefs or assumptions are contradicted by new information.
For many, the belief and wish is that our lives will go back to “normal”. This is highly unlikely, and in order to survive and thrive in this “new normal” we must learn to adapt to our every changing situations.
Our mind is our greatest asset- or liability
Resilience and adaptability
“Psychologists define resilience as the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress—such as family and relationship problems, serious health problems, or workplace and financial stressors. As much as resilience involves “bouncing back” from these difficult experiences, it can also involve profound personal growth.”
Over the past two years many have been able to find equilibrium, balance, and ability to cope. Others did not. Alcohol abuse rose during the pandemic. Suicide was at an all-time high for our youth.
In order to survive and thrive in this new world we need to either have or develop skills that can help us cope. Don’t feel you need to go it alone. There is help. Our mindset is everything in this new world we are seeing unfold. If you or a loved one needs help Mentalhealth.gov has resources to help you or your loved one cope and develop resiliency skills.
Our mind as our friend or foe will make or break us.
Act, don’t react
- Coping with the vast changes around us requires a different way of life, in our interpersonal relationships, how we work, play, eat and travel. We can see the glass as half full or half empty. Develop an attitude of gratitude. It really is up to us. Stay calm, and keep a rational mindset, don’t panic.
- Take, for example, the out-of-control gas prices. For some it is necessary to commute, given the fact that work and daycare are on opposite parts of town. Perhaps your employer would allow you to work a 4 days a week schedule, and either work longer hours or take some work home? That would save on time, gas, and maybe even daycare.
If you are on a bus line, many buses are now equipped with front bike racks. Taking advantage of these racks could offer you a light workout.
Facing out of control grocery bills? Community gardens are a great way to lower your food budget, grow vegies, connect with community, and learn different gardening skills. Contact your local city hall for a list of community gardens in your area.
In addition, microbes in soil are powerful antidepressants. Gardening provides not only food for the body, but food for the soul.
If you are living in and apartment or have limited space, there are some wonderful you tube videos on container and indoor gardening.
- Cyberattacks on our grid and computers are something out of our control, but with a preparedness mindset we can mitigate and not allow these situations to affect us as much as they would otherwise.
- Check your water supply-Cyberattacks can affect infrastructure such as utilities and water supplies.
- Plan on at least 5 gallons of water a day per person. You should have on hand least 2 weeks’ worth of clean, purified water, or a way to purify water. (See previous articles for guidance)
- Food– are you stocked up and do you have easy to prepare food (and can opener)? Do you have way to heat food? Menu planning and utilizing your local USDA ag extension will help keep your grocery costs down and in case of grid down situation you will be equipped to handle this.
- Have activities for all members of the family in case the electric grid and internet goes down. Taking up a hobby such as reading, drawing, string arts, musical instruments.
- Medical supplies, medications, and supplements. Make sure you have ample supply to get you through the most challenging and extended crisis. Talk to your healthcare provider about having extra medications on hand in case of supply disruption.
We will get through this, focus on what you can do and not what you can’t. Even though our way of life is rapidly changing, we can see it as an opportunity for growth.

As the pandemic winds down, more countries are opening their borders to international visitors. The postponed trips to see loved ones, business trips, tourism and medical tourism are slowly becoming a reality. Given a little forethought and planning will make your travel plans go smoothly.
We will cover the following:
- The everchanging landscape of mandates, quarantines, isolation, and vaccinations for each country, can cause confusion surrounding rules and regulations with each country. Do you need to be vaccinated against covid or will a negative covid test do? Quarantine?
- What are recommended medications to bring while traveling?
- How do I travel with medications, especially prescription medication?
- How do I locate medical attention and medication if there is a medical emergency while out of the states?
Covid travel and restrictions
Due to the evolving nature and rules surrounding these questions the CDC travel destinations page has an alphabetical list of countries and their restrictions regarding covid 19 and immunizations. As your planned trip get closer, please check back with this site as the rules frequently change.
When traveling abroad, you are exposed to different germs, time zones, food, and water. A little planning and equipped with the right medications will help make your trip enjoyable and keep you out of a health clinic or hospital in a land where it may be difficult or near impossible to source healthcare.

Medications to Have While Traveling
Note: Many nonprescription medications have interactions and can be dangerous if taken by individuals with prescribed medications or health conditions. As with all medications consult your primary care provider. Follow the hyperlink (to Drugs.com) associated with each medication listed for more information.
Note: As with all drugs, if pregnant, nursing or using with small child always consult your primary care provider for guidance.
- Anti-diarrheal, such as Kaopectate or Pepto Bismol (bismuth subsalicylate) In case of mild diarrhea from contaminated food or water (also known as travelers’ diarrhea) or lack of hygienic practices this medicine is especially important. When traveling, you may not be able to easily locate restrooms. If you are between flights, or in a vehicle where no facilities are available for an extended period of time this medicine can prove to be invaluable. Be sure to stay hydrated while experiencing diarrhea symptoms. Other uses include upset stomach and nausea. If diarrhea continues past a few days or fever present, an antibiotic may be indicated. (See Jase case below)
Note– Do not use if bleeding ulcer, abdominal pain (other than mild cramping) or allergy to aspirin, or with small children. There are drug interactions, check with care provider before using. Do not use more than 2 days or when fever present.
- Laxative/stool softener-Colace 2-in-1 Docusate/senna When traveling across time zones, out of your regular routine, eating strange foods, and limiting liquids while on the road, constipation can strike. A mild laxative with stool softener can help alleviate these symptoms. Be sure to drink plenty of liquids when taking a laxative. Do not use if rectal bleeding or upset stomach are present. Do not take for longer than a week if no bowel movement after one day of use.
- Anti-nausea/motion sickness– Dramamine, (dimenhydrinate) Whether on a cruise, plane, train or traveling by car, motion sickness can ruin a much-anticipated trip. If you are prone to motion sickness, use 30-60 minutes before travel. This medication can cause sleepiness and reduced reflexes as a side effect. There are numerous side effects and interactions and cautions when using this medication. Kidney and liver disease, glaucoma, overactive thyroid, high blood pressure are just a few of the contraindications for use. Do not drive or operate machinery while using.
- Pain reliever, fever reducer, anti-inflammatory– Tylenol (acetaminophen), Advil (ibuprofen) or Aleve (naproxen) Depending on preference- single dose packs of pain relievers. Discuss with your primary care provider which they recommend. Care must be taken with any pain reliever/ fever reducer/ anti-inflammatory. There are many health conditions and medication interactions that can dictate which pain reliever to take. Note: Tylenol is not anti-inflammatory. Advil and Aleve are. There are many differences between the different pain relievers. Tylenol is recommended to take every 4-6 hours (there is a timed release one that is taken every 8 hours), Advil every 6- 8 hours. Aleve is taken every 12 hours, which may be more convenient when traveling, however it is not recommended for small children.
- Antihistamine Benadryl (diphenhydramine) Benadryl has many uses. As an antihistamine it works to help relieve allergic symptoms such as water eyes, sneezing and runny nose. It is also useful as an anti-nausea medication and is used extensively in nursing homes as a sleep aid. Benadryl can cause drowsiness and should not be taken with alcohol. Young children should not take unless recommended by their care provider.
- Jase Case The 5 prescription antibiotics found in this pack can treat many illnesses encountered by travelers. From urinary tract infections to infectious diarrhea to infected wounds to pneumonia and more, this pack of antibiotics can prove indispensable and bring peace of mind. Medical care may be difficult to locate, sourcing the correct medicine to treat symptoms could be even harder. As a prescription medication, travel between countries becomes much easier. The booklet provided covers a wide array of health conditions which will guide you as to whether to take an antibiotic and which one to take if needed.
- Prescription medications and supplements– Make sure your medications are properly labeled and stored correctly. Traveling out of country can present challenges. Be sure to have plenty of medications on hand (at least a week or more) in case of travel delays.
More information when traveling with prescription medications and supplements:
(Taken from the CDC website on travel)
- Make an appointment with a travel medicine specialist or your health care provider to get needed vaccines and medicines at least 4 to 6 weeks before you leave.
- If you plan to be gone for more than 30 days, talk to your doctor about how you can get enough medicine for your trip. Sometimes insurance companies will pay for only a 30-day supply at a time.
- Ask your doctor about any changes to taking your medicine once you’re in a different time zone. Medicines should be taken according to the time since your last dose, not the local time of day.
- Ask how to safely store medicine and check whether it needs refrigeration. Keep in mind that extreme temperatures can reduce the effectiveness of many medicines.
- Pack smart and put your medicines and supplements in your carry-on luggage. You don’t want to be stuck without them if your suitcase gets lost!
- Bring enough medicine to last your whole trip, plus a little extra in case of delays.
- Keep medicines in their original, labeled containers. Ensure that they are clearly labeled with your full passport name, doctor’s name, generic and brand name, and exact dosage.
- Bring copies of all prescriptions, including the generic names for medicines.
- Leave a copy of your prescriptions at home with a friend or relative in case you lose your copy or need an emergency refill.
- Pack a note on letterhead stationery from the prescribing doctor (preferably translated into the language understood at your destination) for controlled substances, such as marijuana, and injectable medicines, such as EpiPens and insulin.
- Check with the foreign embassy of the country you will be visiting or passing through to make sure your medicines are permitted in that country.
-
- Be aware that many countries only allow taking a 30-day supply of certain medicines and require the traveler to carry a prescription or a medical certificate.
- If your medicine is banned at your destination, talk with your health care provider about alternative medicine or destination options, and have your doctor write a letter describing your condition and the treatment plan.
- The International Narcotics Control Board (INCB) provides general information about country regulations for travelers carrying medicines that are made with controlled substances. It’s important to note that INCB may not have information from all countries or territories.
If you must buy drugs during your trip in an emergency, there are ways to reduce your chances of buying counterfeit drugs:
- Contact the nearest US embassy or consulate. They should be able to connect you with doctors and pharmacies that can help you find reliable, quality medicines.
- Buy medicines only from licensed pharmacies and get a receipt. Do not buy medicines from open markets.
- Ask the pharmacist whether the drug has the same active ingredient as the one you were taking.
- Make sure the medicine is in its original packaging.
- Look closely at the packaging. Sometimes poor-quality printing or otherwise strange-looking packaging will indicate a counterfeit product.
A few additional items when traveling
- Water purification tablets these tablets take a few hours to work when added to water but are effective in purifying water polluted with chemicals and bacteria.
- Small bandages for minor cuts and blisters
- Small set tweezers and scissors (may need to check these with luggage)
- Moleskin for prevention and pain relief from shoe friction
- A few packets of oral rehydration solution powder
- Lifestraw water bottle with filter– filters bacteria and chemical pollutants, and are handy when enroute to destination
- Small pack of hand wipes for times when facilities with water and soap are unavailable
- Small packs triple antibiotic ointment
- Small penlight with batteries
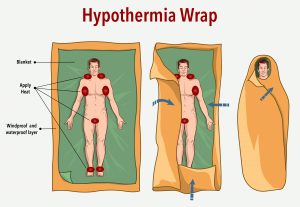
What is hypothermia?
- Hypothermia is caused by prolonged exposures to cold temperatures. When exposed to cold temperatures, your body begins to lose heat faster than it’s produced. Lengthy exposures will eventually use up your body’s stored energy, which leads to lower body temperature. Cold temperatures can be brought on by a number of factors such as ambient air, dampness, water, and wind exposure to name a few.
- Body temperature that is too low affects the brain, making the victim unable to think clearly or move well. This makes hypothermia especially dangerous, because a person may not know that it’s happening and won’t be able to do anything about it.
- While hypothermia is most likely at very cold temperatures, it can occur even at cool temperatures (above 40°F) if a person becomes chilled from rain, sweat, or submersion in cold water. Heat loss to air and water are the most common causes of hypothermia.
In fact, most cases of hypothermia occur when temperatures are between 30 and 50 degrees F. Windy conditions and wet clothes can work together to chill the unaware, even on a summer day. In water temperatures from 70-80 degrees, exhaustion or unconsciousness can set in within 3-12 hours; 60-70 degrees, 2-7 hours, and in water from 50-60 degrees, you could be unconscious in 1-2 hours.
Statistics
Each year there are approximately 700 to 1500 patients in the United States who have hypothermia noted on their death certificate. Adults between the ages of 30 to 49 are more likely affected, with men being ten times more likely than women. However, the true incidence of hypothermia is relatively unknown. Even with supportive in-hospital care, the mortality of those with moderate to severe hypothermia still approaches 50 percent.
Who’s most at risk?
Victims of hypothermia are often:
- Older adults
- Babies sleeping in cold bedrooms
- Small children due to the lower body mass
- People who remain outdoors for long periods—the homeless, hikers, hunters, boaters, people who work outdoors in the elements, etc.
- People who drink alcohol or use illicit drugs.
- In addition to hypothermia from environmental exposure, many medical conditions can cause hypothermia including hypothyroidism, adrenal insufficiency, sepsis, neuromuscular disease, malnutrition, thiamine deficiency, and hypoglycemia (low blood sugar)
- The most common medications that put one at risk for hypothermia are antianxiety drugs, antidepressants, antipsychotics, and opioids.
Symptoms of hypothermia
Adults and children:
- Shivering (in the beginning shivering may be a sign of hypothermia, however it isn’t always present).
- Exhaustion or feeling very tired
- Confusion
- Fumbling hands
- Memory loss
- Slurred speech
- Drowsiness
Babies:
- bright red, cold skin
- very low energy
Hypothermia is a medical emergency. If you notice any of the above signs, take the person’s temperature. If it is below 95° F, get medical attention immediately!
If you are not able to get medical help right away, try to warm the person up.
- Get the person into a warm room or shelter.
- Remove any wet clothing the person is wearing.
- Warm drinks can help increase body temperature, but do not give alcoholic drinks. Do not try to give beverages to an unconscious person.
- Warm the center of the person’s body—chest, neck, head, and groin—using an electric blanket, if available. You can also use skin-to-skin contact under loose, dry layers of blankets, clothing, towels, or sheets.
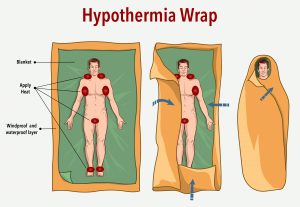
- Get the person proper medical attention as soon as possible.
A person with severe hypothermia may be unconscious and may not seem to have a pulse or to be breathing. In this case, handle the person gently, and get emergency assistance immediately.
- Perform CPR, even if the person appears dead. CPR should continue until the person responds or medical aid becomes available. Keep warming the person while performing CPR. In some cases, hypothermia victims who appear to be dead can be successfully resuscitated.
How to prevent hypothermia
- Dress in loose layers, allowing air trapped between clothing to maintain warmth
- Make sure you are hydrated.
- Eat sufficient calories to maintain body heat
- If caught in an emergency situation don’t eat snow, it will drop your core body temperature. Only drink water or other liquids that are above freezing point
- Small children (and elderly) may not be aware they are cold, always be aware of their clothing- hat, gloves, boots, dry warm socks are essential wear
Frostbite
What is frostbite?
Frostbite is a type of injury to the skin caused by freezing. It leads to a loss of feeling and color in the areas it affects, usually extremities such as the nose, ears, cheeks, chin, fingers, and toes. Frostbite can permanently damage the body, and severe cases can lead to amputation (removing the affected body part).
Who’s most at risk?
Those at risk for frost bite:
- Have poor blood circulation
- Are working outside in the cold
- Are not properly dressed for extremely cold temperatures
- Are exposed to a cold wind chill
- People who have cardiac insufficiency, diabetes and stroke
- Heavy alcohol consumption
What are the signs and symptoms of frostbite?

If you notice redness or pain in any skin area, get out of the cold or protect any exposed skin—frostbite may be beginning. Any of the following signs may point to frostbite:
- A white or grayish-yellow skin area
- Skin that feels unusually firm or waxy
- Numbness to exposed area. Ears, nose, chin, hands, and feet are most at risk for frostbite
A person who has frostbite may not know they have it until someone else points it out because the frozen parts of their body are numb.
If you notice signs of frostbite on yourself or someone else, seek medical care. Check to see if the person is also showing signs of hypothermia. Hypothermia is a more serious condition and requires emergency medical care.
If (1) a person shows signs of frostbite, but no signs of hypothermia and (2) immediate medical care is not available, do the following:
- Get the person into a warm room as soon as possible.
- Unless absolutely necessary, do not walk on feet or toes that show signs of frostbite—this increases the damage.
- Do not rub the frostbitten area or massage it at all. This can cause more damage.
- Put the areas affected by frostbite in warm—not hot—water (the temperature should be comfortable to the touch for unaffected parts of the body).
- If warm water is not available, warm the affected area using body heat. For example, you can use the heat of an armpit to warm frostbitten fingers.
- Do not use a heating pad, heat lamp, or the heat of a stove, fireplace, or radiator for warming. Affected areas are numb and can easily burn.
Don’t substitute these steps for proper medical care. Frostbite should be checked by a health care provider.
The following is an excerpt from the American Association of Dermatology:.
How to prevent frostbite
- Dress in loose, light, comfortable layers. Wearing loose, light layers helps trap warm air. The first layer should be made of a synthetic material, which wicks moisture away from your body. The next layer should be insulating. Wool and fleece are good insulators and hold in more body heat than cotton. The top layer should be windproof and waterproof. A down parka and ski pants can help keep you dry and warm during outdoor activities.
- Protect your feet and toes. To protect your feet and toes, wear two pairs of socks. The first pair, next to your skin, should be made of moisture-wicking fabric. Place a pair of wool or wool-blend socks on top of those. Your boots should also provide adequate insulation. They should be waterproof and cover your ankles. Make sure that nothing feels tight, as tight clothing increases the risk of frostbite.
- Protect your head. To protect your ears and head, wear a heavy wool or fleece hat. If you are outside on a bitterly cold day, cover your face with a scarf or face mask. This warms the air you breathe and helps prevent frostbite on your nose and face.
- Protect your hands. Wear insulated mittens or gloves to help protect your hands from the cold.
- Make sure snow cannot get inside of your boots or clothing. Wet clothing increases the risk of developing frostbite. Before heading outdoors, make sure that snow cannot easily get inside of your boots or clothing. While outdoors, if you start to sweat, cut back on your activity or unzip your jacket a bit.
- Keep yourself hydrated. Becoming dehydrated also increases the risk of developing frostbite. Even if you are not thirsty, drink at least one glass of water before you head outside, and always drink water or a sports drink before an outdoor workout. In addition, avoid alcohol, as it increases your risk for frostbite.
- Recognize the symptoms. In order to detect frostbite early, when it’s most treatable, it’s important to recognize the symptoms. The first signs of frostbite include redness and a stinging, burning, throbbing, or prickling sensation followed by numbness. If this occurs, head indoors immediately.








 Add to
Add to