If you’re considering Jase, chances are you’ve paused and thought, “This makes sense, but I still have a few questions.”You’re not alone. Here are the most common ones we hear, answered plainly. Is this really doctor-prescribed? Yes. Every Jase order is reviewed by a...
Part 2, Common Back to School Illnesses


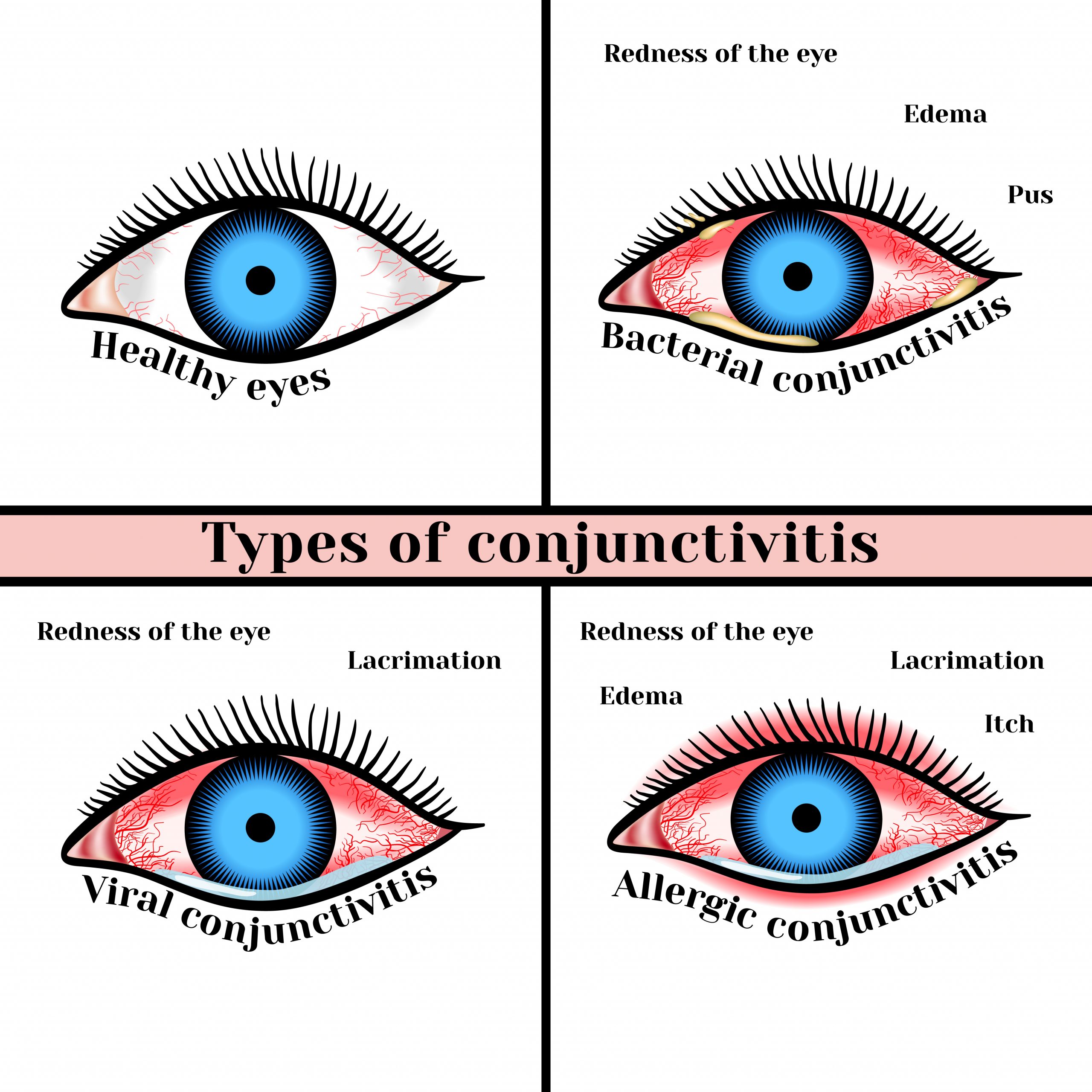
Last week we reviewed head lice, colds and flu and pinkeye. Today we will look at impetigo.
Impetigo
Impetigo is a skin infection caused by one or both of the following bacteria: group A Streptococcus and Staphylococcus aureus. It is the most common skin infection in the age 2-5 group. On occasion adults may become infected, especially if they have another skin issue or are recovering from a cold or other virus.
Group A Streptococcus (group A strep) causes many different infections. These infections range from minor illnesses to very serious and deadly diseases., such as strep throat, scarlet fever, cellulitis, rheumatic fever and more.
Staphylococcus aureus (S. aureus or “staph”) causes skin and soft tissue infections such as abscesses (boils), furuncles, and cellulitis. Most staph infections are not serious, however staph infections can on occasion cause bone, bloodstream, and pneumonia. Methicillin-resistant staph aureus (MRSA) is an antibiotic resistant staph infection is becoming more common.
How impetigo is spread
- Impetigo is highly contagious and can be spread from skin-to-skin contact, like in daycare and school environments where children are in close contact with each other.
- People with scabies or other skin infections or injuries that break the skin are at an increased risk of impetigo.
- Sharing washcloths and towels,
- Contact with sores and rash through personal contact (hugging, playground play)
- Not practicing correct personal hygiene- by keeping sores and blisters clean and removing excess crusty material as it builds up.
Symptoms and diagnosis
- Impetigo starts out as red itchy blisters and sores, that easily spreads when scratched.
- The blisters are filled with yellow or honey-colored fluid and ooze and crust over. Rash that may begin as a single spot but spreads to other areas due to scratching.
- Sores usually start on the face and lips and can spread, arms, or legs and other areas of the body.
- Patches of impetigo on the body (in children).
Treatment
Both S, aureus and group A strep impetigo are treated either with an antibiotic cream or in the case of a severe infection an oral antibiotic.
Your care provider can guide you in the best treatment option available. They may want to take a sample of the bacteria on the skin to determine if you have impetigo, however visual observance is how it is usually diagnosed.
Impetigo can take weeks to clear up. If the rash spreads or does not get better (after a week or so) following treatment, contact your care provider for further guidance. You may need to try another antibiotic.
NOTE: Most impetigo is caused by group A strep
Most cases of impetigo are treated with a prescription antibiotic cream applied directly to the affected area(s). Only severe cases and cases that aren’t healing may need an oral antibiotic.
Be sure to keep sores clean by daily cleansing with mild soap and water and patting dry. Wash soiled washcloths in hot water and dry on high heat. Apply prescribed cream once skin is dry.
It takes about 10 days for sores to appear after someone is exposed to group A strep. If an oral antibiotic is indicated for group A strep impetigo it is usually treated with Amoxicillin-Clavulanate (one of the antibiotics in the Jase case)
If an oral antibiotic is indicated for S. aureus impetigo, your care provider may prescribe doxycycline (one of the antibiotics in the Jase case) or another antibiotic if needed.
Complications of untreated impetigo
Rare complications include:
- Kidney failure
- Glomerulonephritis
- Scarring
Prevention
- Use a clean washcloth and towel each time you wash.
- DO NOT share towels, clothing, brushes, and other personal care products with anyone.
- Avoid touching sores that are oozing. If you do, immediately wash hands, wipe hands on towel and immediately put the towel in the washer or if using paper towels, discard in trash immediately.
- Keep your skin clean to prevent getting the infection. Wash minor cuts and scrapes well with soap and clean water
- Avoid using hot tubs or swimming pools to prevent spread of impetigo to other parts of the body
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
FAQ: Our most commonly asked questions about Jase
Medical Readiness: What Really Kills First
When Disaster Strikes, It’s Not Hunger or Thirst That Takes the First Lives In every disaster zone, from hurricanes in the Caribbean to war zones in Ukraine, the pattern is the same. People worry about food and water, but it’s infection that kills first. A small wound...
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole *Disclaimer: This article is for educational purposes and does not constitute medical advice. Always seek professional guidance.* In the evolving...