Don't let allergies turn into something more serious!It’s that time of year. The weather is lovely, the flowers are in bloom, the birds are chirping, and the tissues are flying? Summer’s around the corner, and Spring is certainly in the air, but so are the allergens....
Men: Lose the Stigma, Regain Your Health

The stigma that surrounds mental health, especially when it comes to men has created a vacuum of silence. With all the awareness of mental health and services nowadays, men still don’t seek help in this arena.
Societal norms of masculinity, embarrassment and shame are some of the reasons men are less likely to seek help. Many view seeking help as a sign of weakness, and continue to try to cope with depression, anxiety and feelings of hopelessness on their own. Terms such as “unmanly” or “weak” are hold an undercurrent of negative connotation of what it means to be a man. In general, many men tend to hide their feelings from their family, putting on a false front that nothing is wrong but inside angst and inability to cope with these feelings can lead to destructive and unhealthy behavior.
Unhealthy ways of dealing with stress lead to physical and emotional destruction

Job pressure (or unemployed), stressful family relations, and social isolation, if not dealt with in a healthy manner can lead to serious health problems. The buildup of stress hormones – the fight or flight mechanism that is designed to charge your muscles and entire nervous system with the energy to flee or fight a perceived danger can turn on itself if you aren’t able to effectively deal with the situation or have a physical outlet for all the stored-up energy. This mechanism was lifesaving back when life’s stressors were tied to survival- a bear attack, natural disasters that required rescue of a loved one or even hunting. In today’s modern world, these real life dangers and scenarios are not part of our daily lives. Stress nowadays is usually tied to our sedentary lifestyle. We ae unable to flee or physically fight the opponent. Because of this new ways of coping have to take place. If not, built up stress can lead to heart disease, cancer and even suicide. It is a widely known fact that stress,-or how you deal with it- is the leading cause of heart disease and cancer, which are the top two causes of death in men.

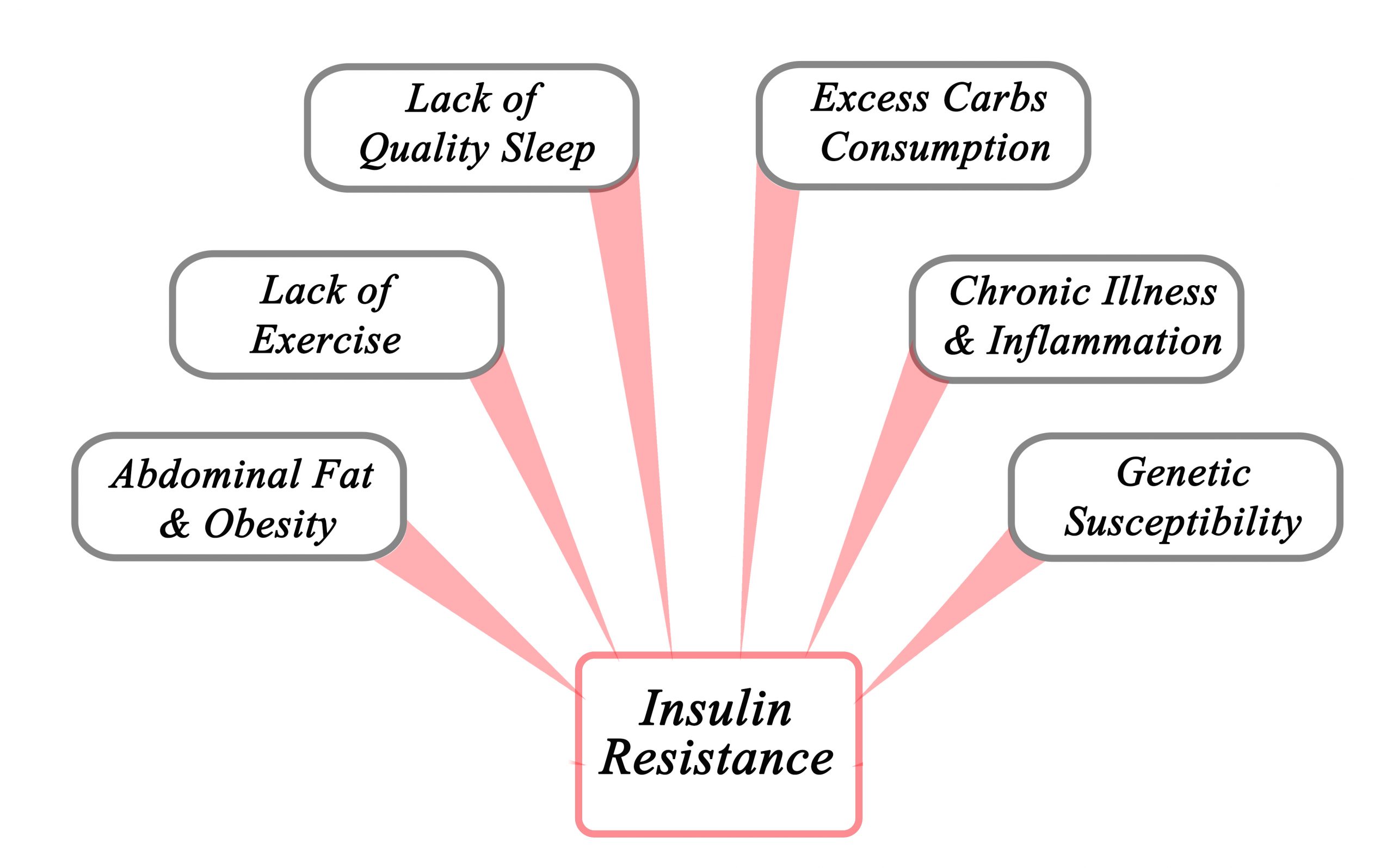
The fight or flight response to stress that isn’t dealt with can lead to anger outbursts, self-destructive behavior, feelings of helplessness, anxiety, depression and isolation from friends and family. Lack of exercise, unhealthy diet, alcohol, and substance abuse can snowball into more depression (alcohol is a depressant).
This same fight or flight response is responsible for the majority of deaths in men- increased cortisol levels from untreated stress, along with decreased immune function set the stage for the two most common causes of death in men- heart disease and cancer. If there is no outlet for stress, the body’s stored up adrenaline will literally take your body hostage.
Make your health a priority.
3 steps towards effectively dealing with stress

- Acknowledge your stress. If you haven’t already, take time out to figure out what is bothering you. Seek counselling or a trusted friend/ relative to confide in. There may be multiple stressors in your life. Stress can be anything- from long commutes in traffic, demanding work situations, demands- both reasonable and unreasonable from family and friends to an unexpected health crisis. Along with counselors, friends, and trusted family members to confide in, many find keeping a journal a good way to identify and keep track of events that trigger stress response.
- Plan. Make that counselling appointment or schedule time to talk with a trusted friend or family member and follow through. Many times, excuses and commitments get in the way of doing this. Schedule time as if it was an appointment- which it is-n appointment towards health and wellbeing. Make or keep doctors’ appointments. This is especially important if you haven’t seen your care provider for a while. High blood pressure is known as the silent killer. Many times, there are no symptoms until a fatal heart attack hits. Lifesaving medications may be prescribed to treat high blood pressure or other stress related diseases.

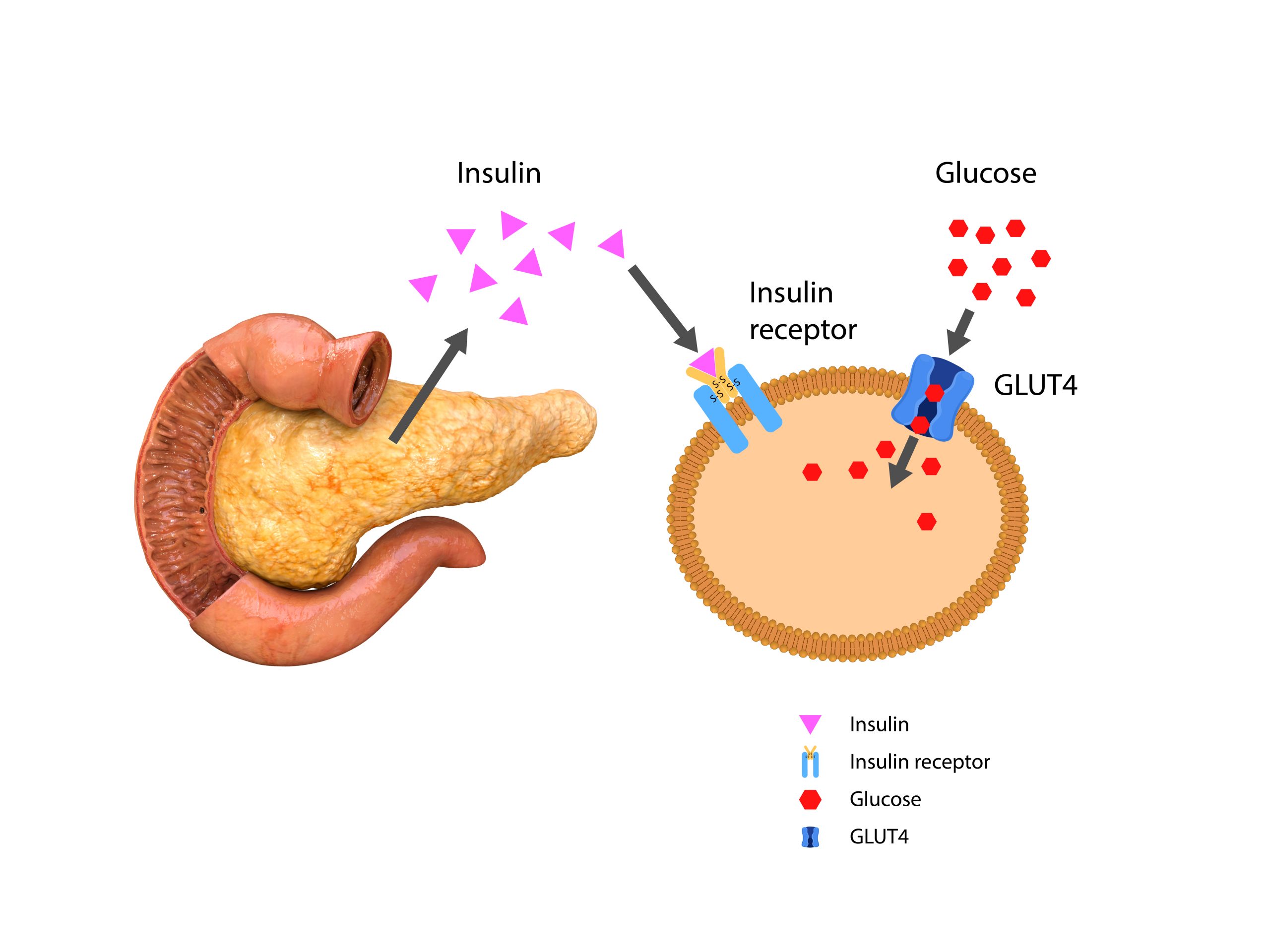
3. Once you have identified the stressor(s), remove the stress from your life. If you are unable to change the situation, find healthy ways to cope with it. Channel the excess energy through physical activity by joining a gym, running, hiking or a hobby that brings you enjoy. Maintain a healthy diet. Cut out alcohol if you are currently using it to cope with life’s stressors. Join an AA meeting if alcohol abuse is a problem. Meditation, deep breathing and refocusing can go a long way toward stress reduction. In addition, make sure you keep up with your annual doctor’s appointments. Your doctor may prescribe medication-either short term or long term to help cope with stress. In addition, some diseases go undiagnosed that can cause depression such as diabetes.
Life has become challenging in ways our ancestors never dreamed. Our world is constantly changing-more so in recent years than at any other time in history. It is easy to put off self-care while putting out life’s fires. However, by neglecting your own needs you set could be setting yourself up for long term health crises.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
Allergy Season and the Risk of Respiratory Infections
Ten Ways Parents Can Improve Their Child’s Health Today
Small changes can make a big difference!As parents, there's nothing we want more than for our children to be healthy and happy. We dream of them skipping through life with boundless energy, tackling new adventures with enthusiasm, and growing into strong, confident...
Stop Ticks in Their Tracks: Prevention, Removal, and Treatment
Don't get ticked off: Tips for how to conquer those tiny terrors.Unfortunately we humans aren’t the only ones who enjoy the nice weather this time of year. Ticks usually go dormant for the winter (unless they have found a warm, hospitable host), so we tend to let our...