There are a lot of things we like to stock up on: pressure-canned fruits and vegetables, canned goods at the grocery store. (“Two for a dollar?! I need another cart!”), soaps and cleaners . . .And toilet paper! Oh yes! But stock up on prescription medicines for months...
The Overlooked Vital Sign
As long as man has walked the earth, pain has been part of life.
Pain is defined as a localized or generalized unpleasant bodily sensation or complex of sensations that causes mild to severe physical discomfort and emotional distress and typically results from injury or disease. It is a complex mechanism that alerts us to injury or illness. Pain isn’t a pleasant experience; however, it can save your life.
Why is pain called the 5th vital sign?
In 1995, Dr. James Campbell addressed the American Pain Society urging that health care providers treat pain as the “fifth vital sign” (The other vital signs are blood pressure, heart rate, temperature, and respiratory rate.) highlighting the need for improved pain care. The tide has turned for the better. Historically, care providers hadn’t adequately managed pain. It is now considered a very important part of a patients assessment and well-being.
Pain can be both physical and psychological. In fact, physical and psychological pain share the same neuro mechanisms and the same regions of the brain where these processes take place. In addition, both physical and psychological pain stems from inflammation and the inflammatory response.
Physical pain-acute and chronic
Acute pain- Acute pain comes suddenly, can be severe and resolves over a short period of time (within a month or so). Injuries, illnesses (such as sore throat), labor and childbirth, dental work, are classified as acute pain.
Chronic pain- Chronic pain is pain that lasts a sustained period, usually lasting 3 or more months. Examples are arthritis, bone healing after break, cancer, back pain, fibromyalgia, autoimmune diseases. Chronic pain can cause tense muscles, lack of energy, depression, and anger, which can lead to psychological pain. An estimated 35-45% of chronic pain sufferers experience depression.
Psychological pain- Rejection, loss of a loved one, loss of job or health and chronic pain are a few ways psychological pain can manifest. These emotions (anger, depression, rejection, loss) can trigger inflammation, which in turn can cause psychological pain. Which then manifests as physical pain.
Assessing pain-verbal and nonverbal/physical cues
Seek medical attention if experiencing abdominal pain, pain from an injury, trauma, pain for unknown causes or a fever for unknown reasons.
Depending on the age and mental capacity of the patient, pain can be expressed in either verbal, nonverbal/physical. Young children, infants, and patients with cognitive deficits (Alzheimer, autistic) won’t be able to adequately report pain. It is important to assess the person’s ability to accurately express their pain. Dementia patients may state they aren’t hurting; however, their body language may reveal otherwise. The same goes for young children. Nonverbal cues should be relied on in these groups. Observe and evaluate.
Verbal expressions- Yelling, crying, tears, hyperventilating, stating they are in pain, moaning, calling out for help are examples of verbal expressions of pain.
Ask:( Verbal patients with no age related (young children and infants) or cognitive impairment)
- Type of pain? Stabbing, burning, aching, dull, throbbing sharp, cramping?
- Location (is there more than one place)
- Duration/activity- How long has it hurt? Does the pain come and go? Is there pain with specific activity- are there activities that make the pain worse? Are there any activities or postures that provide pain relief?
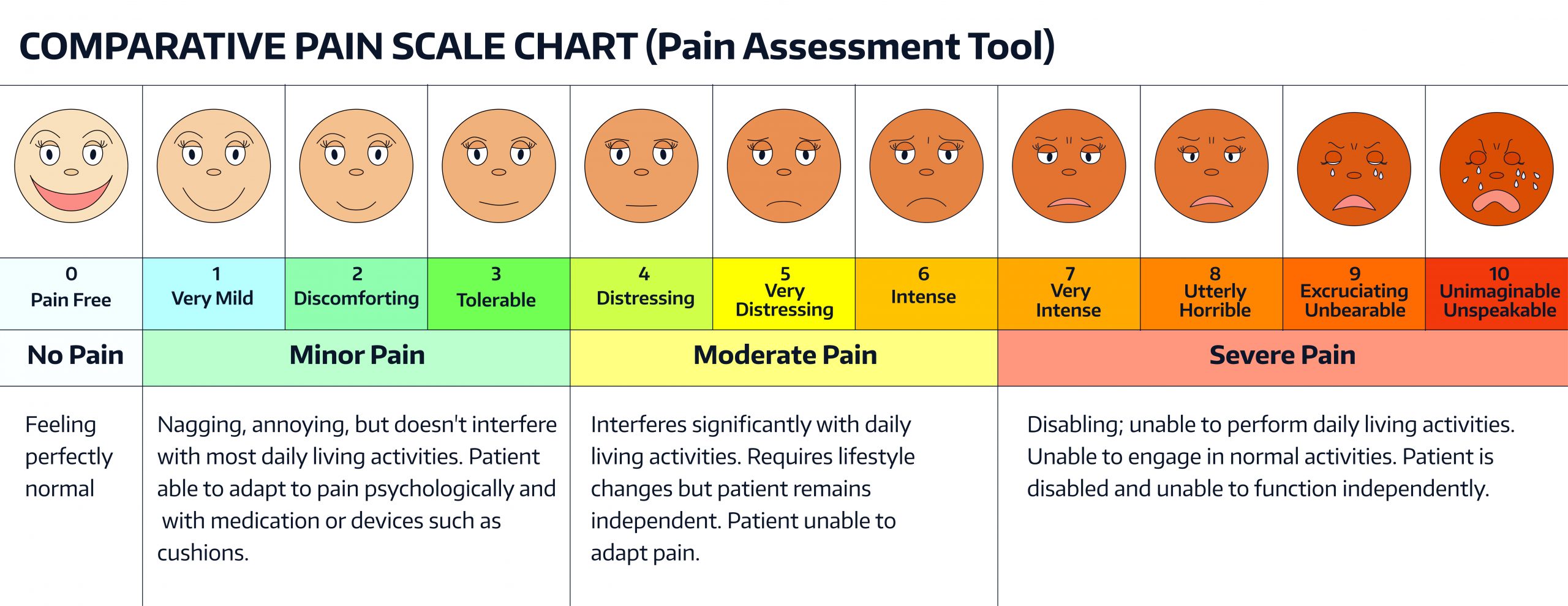
Use the pain scale assessment to determine severity of pain
Nonverbal/physical- Some nonverbal expressions of pain include facial expression of pain, altered gait/limping, rubbing a body area, tense tone/rigidity, decreased movement, guarding a part of the body that is hurting, pacing, rocking, fidgeting, increased heart rate and blood pressure, sweating. This type of assessment will be necessary when working with nonverbal patients and very young children.
Infants pain communication
Infants- Since infants can’t tell you when they are in pain, it is very important to know the signs of distress/pain.
- They may cry or whimper and be unable to settle.
- They may be tense, with clenched fists and may keep their arms and legs close to their chest.
- They may be fidgety, agitated or have a disturbed wake / sleep schedule.
- They may be pale, flushed or sweaty.
- They may shut their eyes tightly, furrowing their eyebrows or have larger than normal pupils.
The NIH has developed a neonatal/ infant pain scale, which can be accessed here. This is a handy tool to help determine your child’s level of distress/pain.
Interventions
(Always check with your care provider if the pain is excessive, unknown in origin and before taking any over the counter medications)
Pain scale
Utilize the pain scale assessment tool. Have them point to which face they feel best describes how they are feeling or use the 1-10 severity of pain level tool.
Medication
Since pain causes inflammation, anti-inflammatory drugs such as ibuprofen and naproxen can help. Pain can cause muscles to tense (guarding) which can make the pain worse. Talk to your care provider about therapies or drugs that may help with this.
Nonpharmacological interventions to relieve pain
Both acute and chronic pain sufferers can benefit from several therapies to relieve pain.
Some of these therapies/interventions are:
- Accupuncture– involves the insertion of extremely fine needles into the skin at specific “acupoints.” This may relieve pain by releasing endorphins, the body’s natural pain-killing chemicals, and by affecting the part of the brain that governs serotonin, a brain chemical involved with mood.
- Companionship can relieve anxiety and take the focus off the pain.
- Positioning to relieve pain.
- Hot/cold therapy Depending on the type of pain (injury or cramp, for instance) heat or cold can be a powerful tool to alleviate pain.
- Massage therapy- Especially effective if tense from pain.
- Meditation/prayer can calm the mind and body.
- Relaxation/guided imagery positive, guided imagery is beneficial by allowing the body to relax-check out this video on guided imagery
- Deep breathing exercises- check out this video on deep breathing to reduce pain.
- Transcutaneous Electrical Nerve Stimulation (TENS) is a procedure in which electrodes, placed on a person’s back, give off an electric signal that stimulates nerve cells through the skin. The numb-like feeling that results. It can help some people overcome pain. TENS blocks pain messages to the brain and modifies pain perception.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
Why Do People Want a 12-Month Supply of Their Prescription Medications?
Navigating Spring’s Waters: Hydration, Recreation, and the Risk of Giardia
Even crystal clear water can conceal hidden hazards. .Spring Brings water, water brings risks. With spring in full swing and temperatures rising, our thirst (pun intended) for water grows as well. This applies to both the need to stay hydrated and the desire to cool...
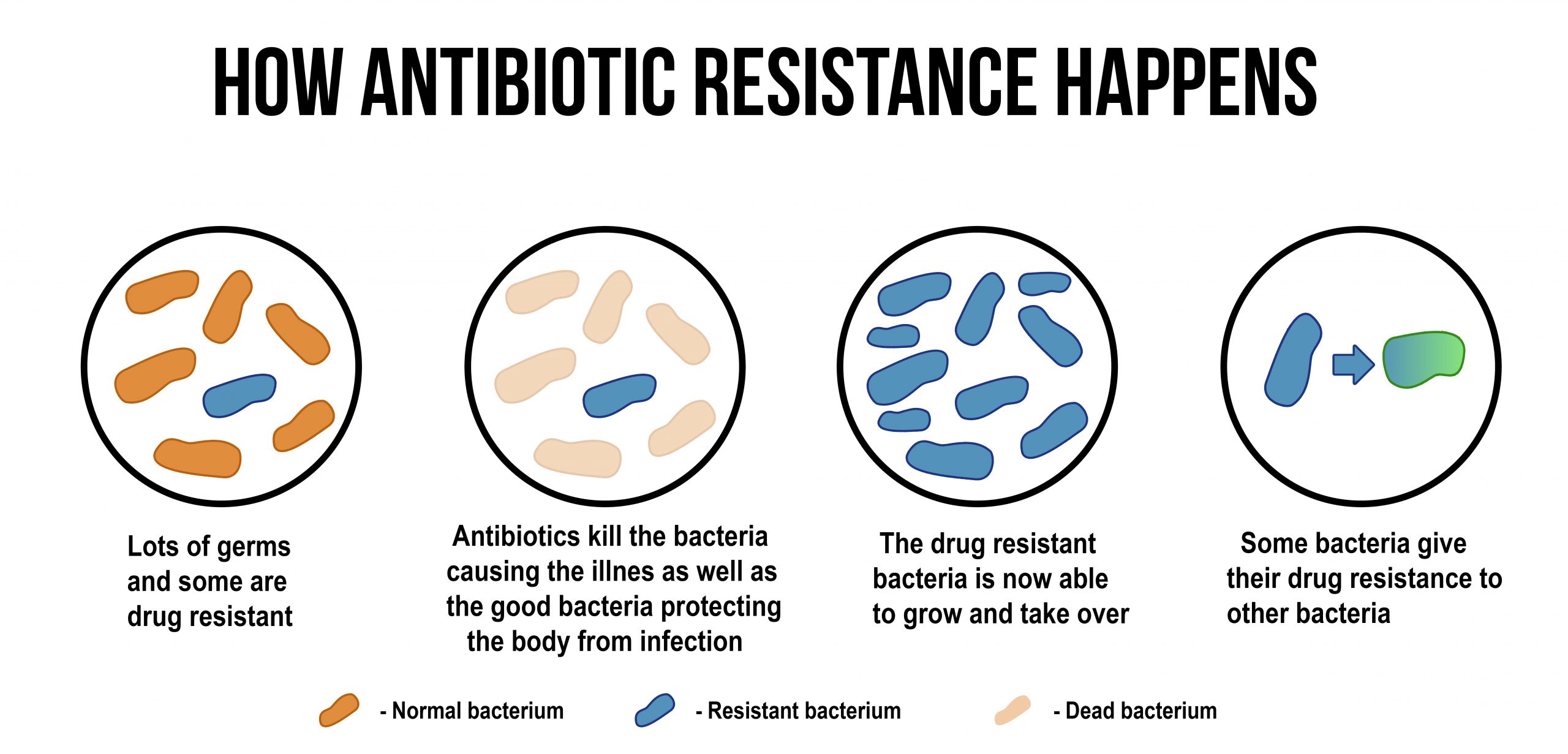
The Importance of Timely Antibiotic Intervention
Accelerate healing through early treatment. .The Key to Effective Infection Management: Early antibiotic intervention and at the right dose. While aggressive antibiotic treatment with high dosages has been the go-to methodology of treatment historically, research by...