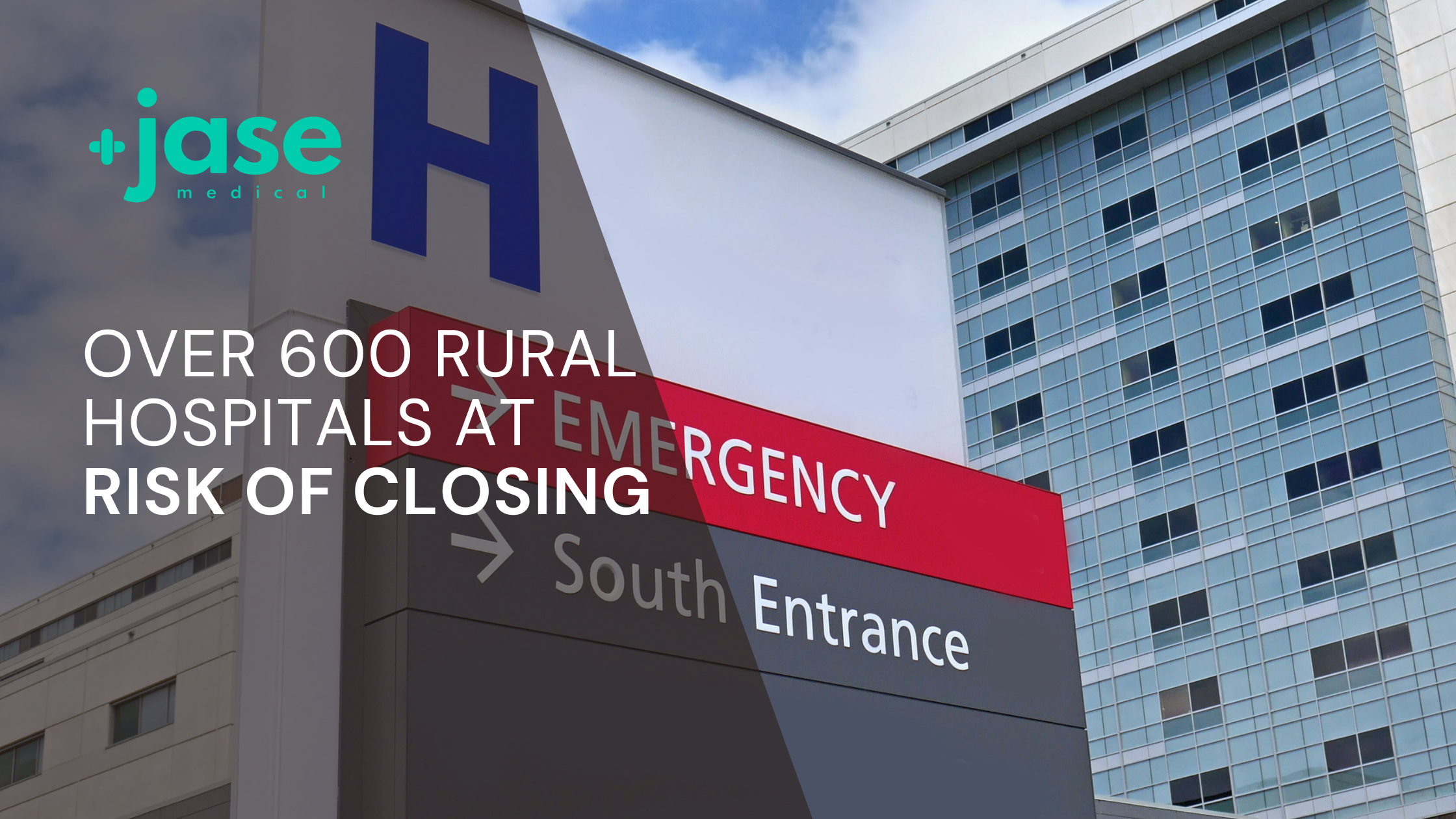
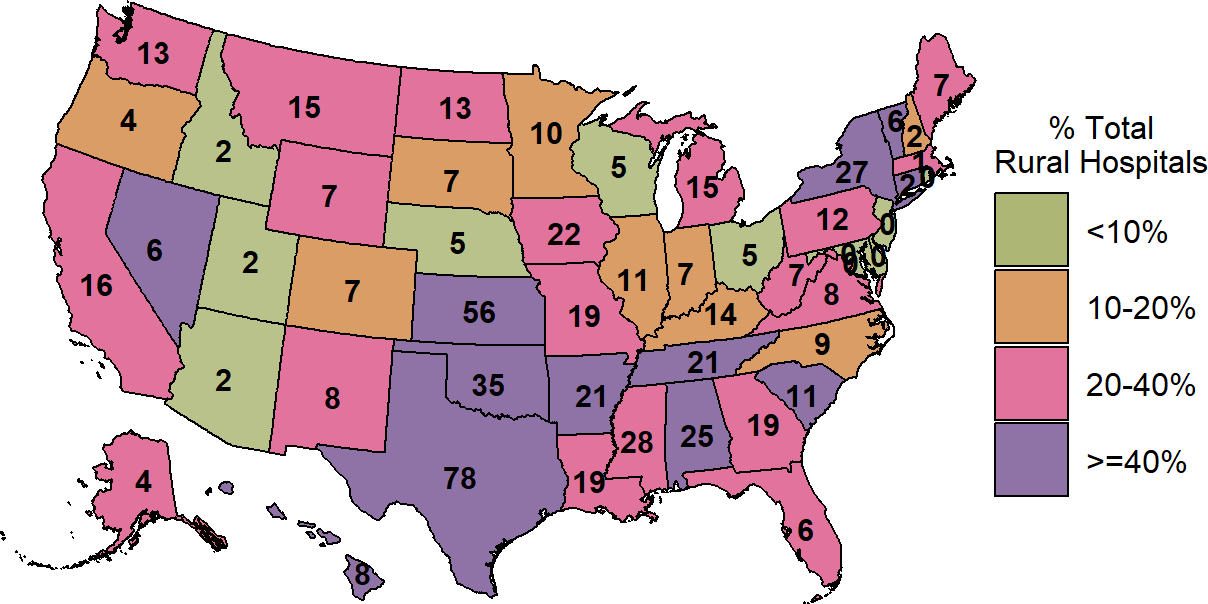
Throughout the nation many rural hospitals are on the brink of closure, citing physician shortages and lack of adequate funding to keep their doors open. A report from the Center for Healthcare Quality and Payment Reform (CHQPR) revealed that more than 600 rural hospitals – nearly 30% of all rural hospitals in the country – are at risk of closing in the near future.
These hospitals are not just emergency rooms, many are the anchor for primary care, rehabilitative therapies, labs and x ray departments and maternity care. If the hospital closes many , if not all, other rural healthcare services in the area will also disappear.
Lack of adequate revenue
Rural hospitals and clinics are forced to operate many times at a loss- not because they are inefficient but because they have the same overhead as their urban counterparts.
ER staffing 24/7- Urban hospitals have more patients coming through their doors than their rural counterparts. Even though both require adequate round the clock staffing, the volume of patients in urban areas offsets the overhead.
There are over 1,000 small rural hospitals, representing more than 25% of all the short-term general hospitals in the country, but they receive only 2% of total national hospital spending.
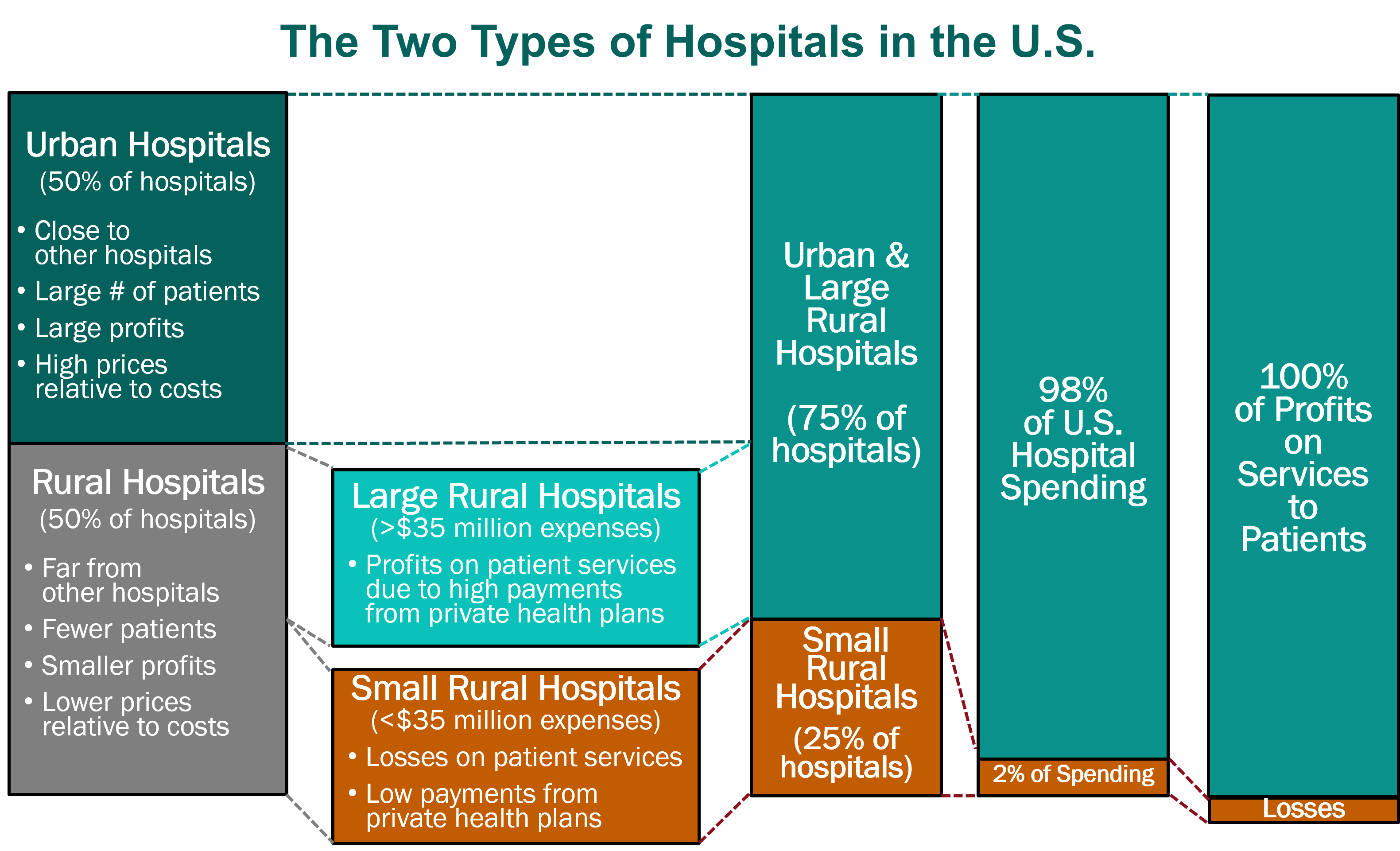
Insurance reimbursement disparity
A recent report by Center for Healthcare Quality and Payment Reform (www.CHQPR.org):
“A common myth about rural hospitals is that most of their patients are on Medicare and Medicaid. In fact, about half of the services at the average rural hospital are delivered to patients with private insurance (including both employer-sponsored insurance and Medicare Advantage plans). Low margins or losses on patients with private insurance, combined with losses on Medicaid and uninsured patients, can force small rural hospitals to close.”
Physician shortage
According to NHRA (National Rural Health Association)
“Ease of access to a physician is greater in urban areas. The patient-to- primary care physician ratio in rural areas is only 39.8 physicians per 100,000 people, compared to 53.3 physicians per 100,000 in urban areas. This uneven distribution of physicians has an impact on the health of the population.”
Some reasons cited for the rural physician shortage are long hours, lower reimbursement of insurance compared to urban areas, aging population of physicians that are nearing retirement, managing patients with higher proportion of chronic illnesses (diabetes, coronary heart disease) and lifestyle of rural living.
Rural hospitals and clinics serve farmers, ranchers, and others that provide food and services for the entire nation. Many of the nation’s natural resources- coal mines, oil and natural gas production are in these areas. Rural hospitals and clinics also provide care for visiting tourists to national parks and outdoor recreation if an emergency arises. If this population can’t continue to live and work in rural areas because of lack of medical services, the entire nation will suffer.
Solutions
- Match reimbursement with cost of doing medicine
Current insurance reimbursements are below cost of delivering care. Saving Rural Hospitals states that increasing spending to meet cost of services (total would be 4 billion annually) could help offset the financial losses. This sounds like a lot of money, however this amounts to only 1/10 of 1% of total national healthcare spending, which is more than $1.3 trillion spent on all urban and rural hospitals in the country.
- Telemedicine
Rural communities could benefit from telemedicine, which solves the problem of rural patients having to drive long distances (sometimes over 70 miles) to see a doctor or consult with a specialist. Telemedicine can treat chronic conditions and provide a preventative approach to healthcare not usually found in rural areas.
- Establish more rural residency programs and mentoring opportunities. As more rural physicians enter retirement age they are ideally positioned to mentor and support new physicians in rural medicine.
- Utilize midlevel providers to offset the long hours the physician faces along with providing care more economically. Midlevel providers- nurse practitioners and physician assistants- are a more economical way to support the physician and can provide relief from long hours faced by rural physicians.
Until such a time that above solutions can be implemented, anyone living in rural areas should consider the very real possibility that their local hospital could be shut down in the near future. Are you prepared for such an event?
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
FAQ: Our most commonly asked questions about Jase
If you’re considering Jase, chances are you’ve paused and thought, “This makes sense, but I still have a few questions.”You’re not alone. Here are the most common ones we hear, answered plainly. Is this really doctor-prescribed? Yes. Every Jase order is reviewed by a...
Medical Readiness: What Really Kills First
When Disaster Strikes, It’s Not Hunger or Thirst That Takes the First Lives In every disaster zone, from hurricanes in the Caribbean to war zones in Ukraine, the pattern is the same. People worry about food and water, but it’s infection that kills first. A small wound...
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole *Disclaimer: This article is for educational purposes and does not constitute medical advice. Always seek professional guidance.* In the evolving...