As summer winds down and focus on starting a new school year is right around the corner, many parents and children are getting ready- adjusting bedtimes, school lunches, transportation to and from school, and in some instances, starting a new school. Along with this,...
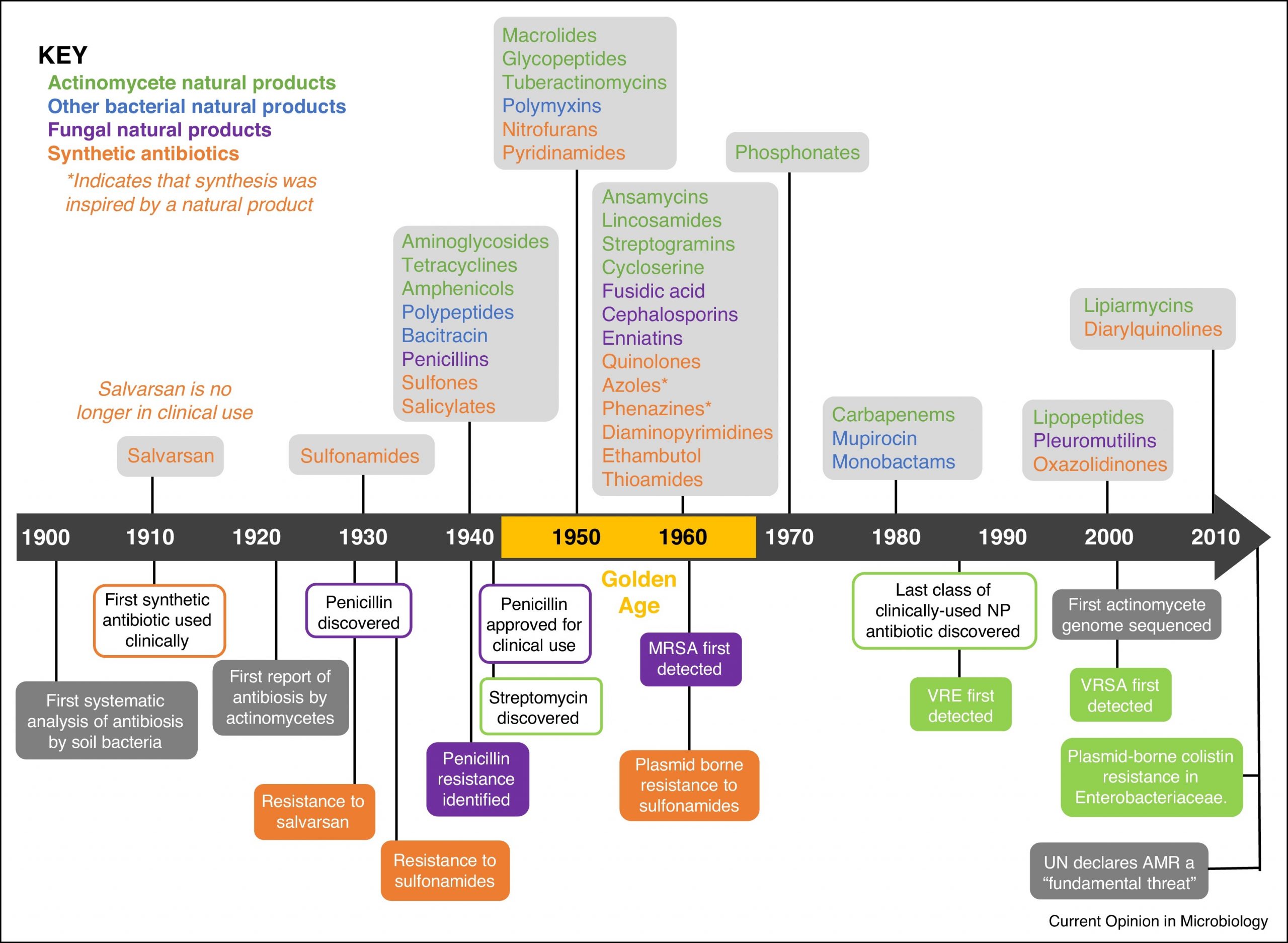
How do Antibiotics Work? Part 2

In part 1 the history of antibiotics and how they work was reviewed. This week we will look at
- The role of biofilms in bacteria and why these present a challenge to our modern-day arsenal of antibiotics
- Antibiotic resistance challenges
The role of biofilms in bacteria and why these present a challenge to our modern-day arsenal of antibiotics
What are biofilms?
It wasn’t until the 1970s that biofilms were found to play a role in bacterial infections in cystic fibrosis patients. Bacterial biofilms are clusters of bacteria that are attached to a surface and/or to each other and embedded in a self-produced matrix of fibrin like proteins or polysaccharides.
The matrix attaches to a surface and manufactures a slimy substance that offers protection that live within the biofilm. This substance is called the Extracellular Matrix (ECM)
The ECM matrix includes proteins, polysaccharides, glycolipids, glycoproteins, and DNA. There can be more than one bacterium or microbe in the matrix which can transfer genetic material between them. This promotes adaptation of the microbes.
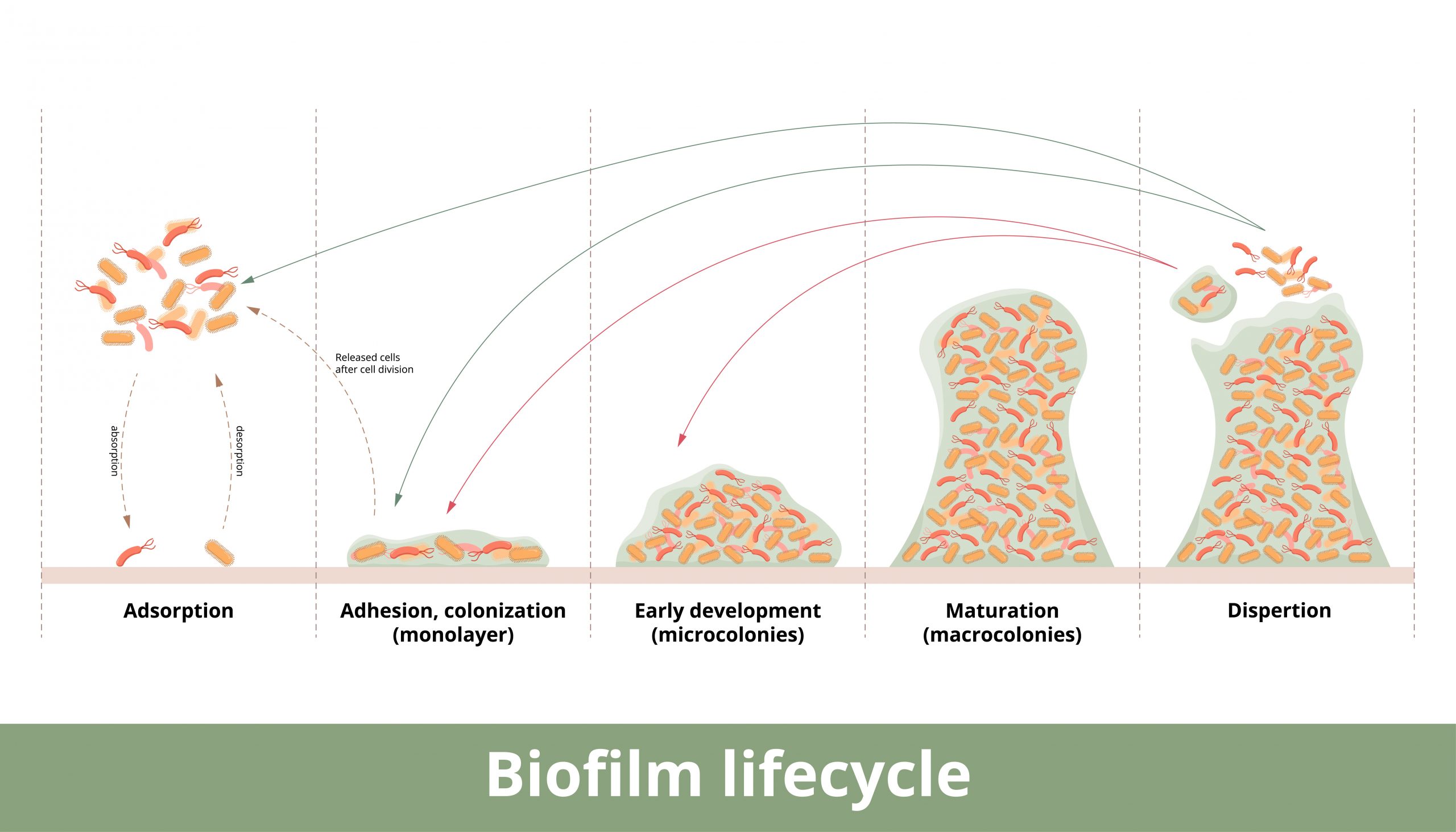
For instance, Staphylococcus aureus can form biofilm in four different ways- from polysaccharides to protein/DNA to fibrin to amyloid biofilms. The biofilm protects the bacterium from penetration of any invasive substances that would kill it. This can make the bacteria highly resistant to antibiotics where it can hide within this matrix and can re emerge after antibiotic therapy to reinfect the host.
The National Institutes of Health (NIH) revealed that among all microbial and chronic infections, 65% and 80%, respectively, are associated with biofilm formation. Of note is that biofilms can form on living and nonliving surfaces such as indwelling catheters, implanted medical devices, and protheses.
Common bacteria associated with Biofilm
Staphylococcus aureus
The most common infection associated with implants and medical devices. These devices are very susceptible to biofilm infection. Removal of the implant or device can help bring the infection under control in some instances, however some bacteria are usually dislodged upon removal and take up residence in other parts of the body.
Pseudomonas aeruginosa
According to PubMed “Pseudomonas aeruginosa is an opportunistic human pathogen causing devastating acute and chronic infections in individuals with compromised immune systems. Its highly notorious persistence in clinical settings is attributed to its ability to form antibiotic-resistant biofilms.” It is found in both indwelling medical devices, catheters, ventilators and in humans.
P aeruginosa is also a major cause of hospital acquired infections, ranging from ventilator associated pneumonia to cystic fibrosis patients succumbing to this infection and diabetics with non-healing ulcers.
Escherichia coli
A major cause of urinary tract infections and can be difficult to eradicate.
Biofilm-associated diseases of different body systems and their affected organs.
Some of the more common biofilm associated diseases include:
- Otitis media- ear infection
- Cardiac valve-Infective endocarditis
- Arteries- Atherosclerosis
- Salivary glands- Salivary duct stones
- Gastrointestinal tract- Inflammatory bowel disease and colorectal cancer
- Skin and underlying tissue- Wound infections
- Vagina- Bacterial vaginosis
- Uterus and fallopian tubes- Chronic endometritis
- Mamary glands- Mastitis
- Nasal cavity and paranasal sinuses- Chronic rhinosinusitis
- Throat, tonsils, adenoids, larynx and vocal cords- Pharyngitis and laryngitis
- Respiratory- Upper and lower airways- Cystic fibrosis, pseudomonas pneumonia
- Mouth- dental caries
Antibiotic resistance challenges
As we enter a world where antibiotic resistance becomes more commonplace there are a few measures we can take to help alleviate this.
The 4 Rs of home antibiotic therapy:
- Right person- don’t share antibiotics
- Right route- by mouth, injection or topical
- Right time- and how often to take
- Right dose- don’t skip or save antibiotics, finish entire course of therapy
Research points to taking low doses of or not completing antibiotic therapy can cause antibiotic resistance- the pathogenic (disease causing) bacteria aren’t all the way eradicated. This, in turn allows the bacteria time to mutate and develop resistance to the antibiotic.
- Use antibiotics appropriately
Antibiotics treat bacteria and, in some cases, parasitic and fungal infections. They do not treat viruses. Overuse and not used appropriately has led to antibiotic resistance. This in turn forces the practitioner to use stronger antibiotics with more side effects.
- Biofilm disruptors
Combination drug therapies are sometimes used to combat biofilm.
There is a growing body of evidence that some spices and foods can act as biofilm disruptors, allowing antibiotics to reach the pathogenic bacteria. One is turmeric. Others include oil of oregano and cranberry, used in urinary tract infections.
- Brooke Lounsbury
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
After School and Home Alone – Do Your Children Know What to do in an Emergency?
How Long Do My Meds Last? A Look at Azithromycin
(They may last longer than you think)Azithromycin is a type of macrolide antibiotic. It works by decreasing the production of protein and stopping bacterial growth. Other macrolide antibiotics include clarithromycin and erythromycin. Because of the anti-inflammatory...
Jase Founder Dr. Rowland Deploys with Aerial Recovery Group to Lahaina
When Dr. Shawn Rowland heard of the fire in Lahaina, and thousands were displaced, he wanted to offer his home on nearby Oahu for a displaced family or two to stay. He had no idea that he would be a part of the rescue and recovery efforts of a global outreach group...