If you’re considering Jase, chances are you’ve paused and thought, “This makes sense, but I still have a few questions.”You’re not alone. Here are the most common ones we hear, answered plainly. Is this really doctor-prescribed? Yes. Every Jase order is reviewed by a...
What is Insulin Resistance?

To understand what insulin resistance is, we first need to look at what insulin is and what it does.
Insulin is a hormone that is secreted by beta cells of the pancreas. The pancreas is located under the left rib cage and extends slightly to the right. The pancreas releases insulin in response to consuming carbohydrate rich foods, especially when high in simple sugars.
The lock and key gatekeeping loop
Once insulin is released into the bloodstream, it travels to cells throughout the body where it binds to special cell receptors called glucose transporters. These cell receptors act as the gatekeeper for glucose to enter the cells. Once insulin binds to these receptors it “unlocks” the cell, allowing glucose to enter the cell, providing energy for the cell. Depending on what part of the body they are located in, there are 14 different glucose transporters that have been identified. These transporters are responsible for signaling the pancreas to stop releasing insulin when no longer needed. This is called a feedback loop.
The image below shows how one of the receptors does its job- GLUT4 transport receptor
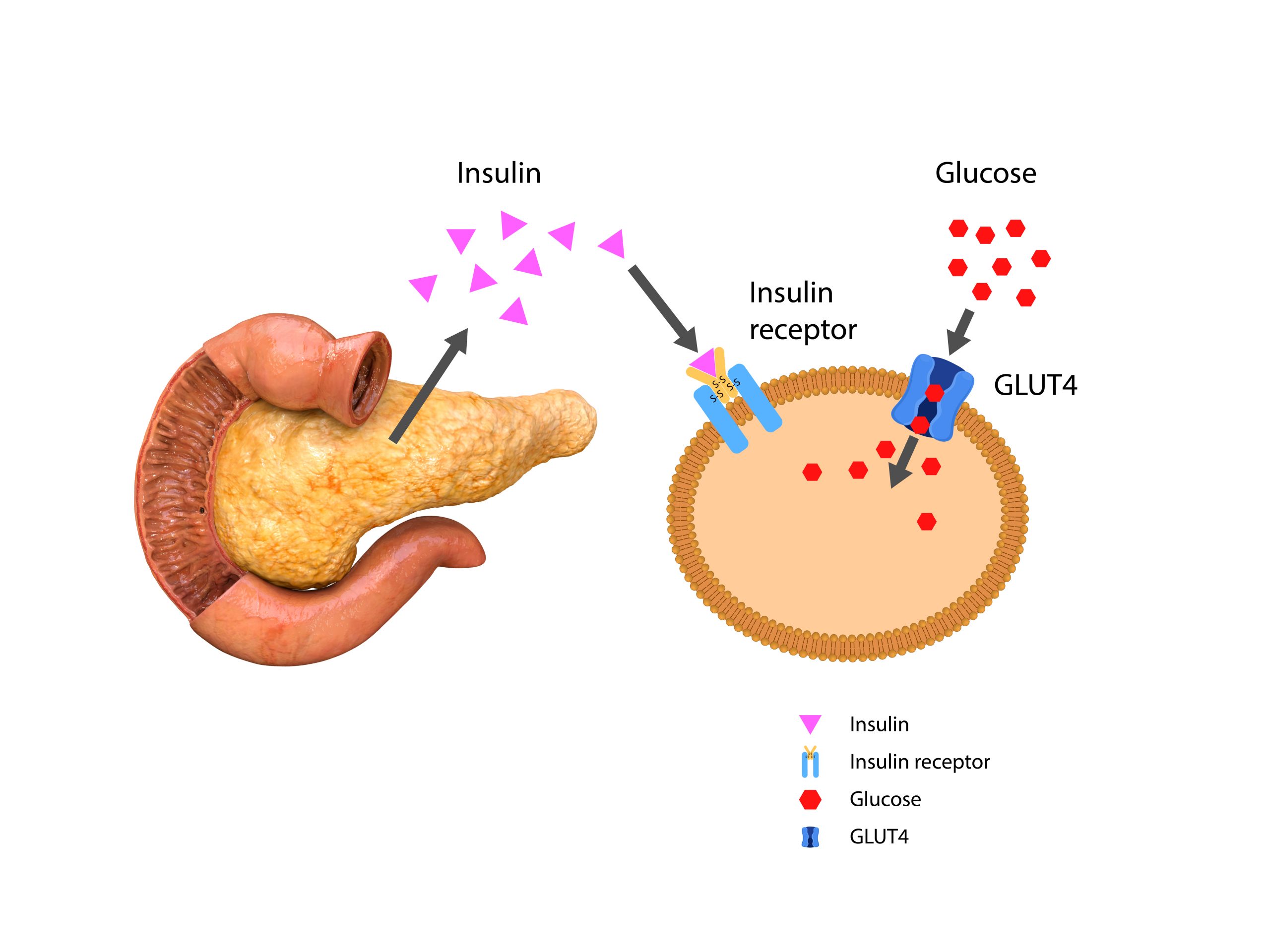
Defective or decreased insulin receptors causes insulin resistance (AKA impaired insulin sensitivity).
Mild insulin resistance (fasting glucose of 100–125 milligrams per deciliter and/or an A1C of 5.7% to 6.4%) is usually caused by decreased insulin receptors. This is also called prediabetes. About 34% of middle-aged adults in the U.S. fall in this category.
Severe insulin resistance, also known as type 2 diabetes, (fasting insulin levels above 50–70 μU/mL or levels that exceed 350 μU/mL after an oral glucose tolerance test) is caused by both decreased insulin receptors and defective receptors.
The development of insulin resistance typically increases insulin production (hyperinsulinemia) so your body can maintain healthy blood sugar levels. Elevated levels of insulin can result in weight gain, which, in turn, makes insulin resistance worse.
When blood glucose is excessive, the body converts it into glycogen where it is stored mostly in muscle and liver for energy when glucose isn’t readily available. When the glycogen stores are needed, enzymes release and convert the glycogen back to readily available glucose for the cells to use.
Signs of insulin resistance
(In addition to high insulin levels, and elevated blood glucose testing levels)
There is no definite test for insulin resistance that is affordable and easy to test– most testing is done in research facilities. Instead, practitioners rely on a series of labs to determine insulin resistance.
- High triglyceride levels.
- High LDL (bad cholesterol)
- Low HDL (good cholesterol)
- Hardening of the arteries (atherosclerosis)
- High blood pressure (hypertension)
- Metabolic syndrome or insulin resistance syndrome is a group of conditions- obesity, high blood pressure, high blood triglycerides, low levels of HDL cholesterol and insulin resistance that raise your risk of coronary heart disease, stroke, and other serious complications.
Causes of insulin resistance
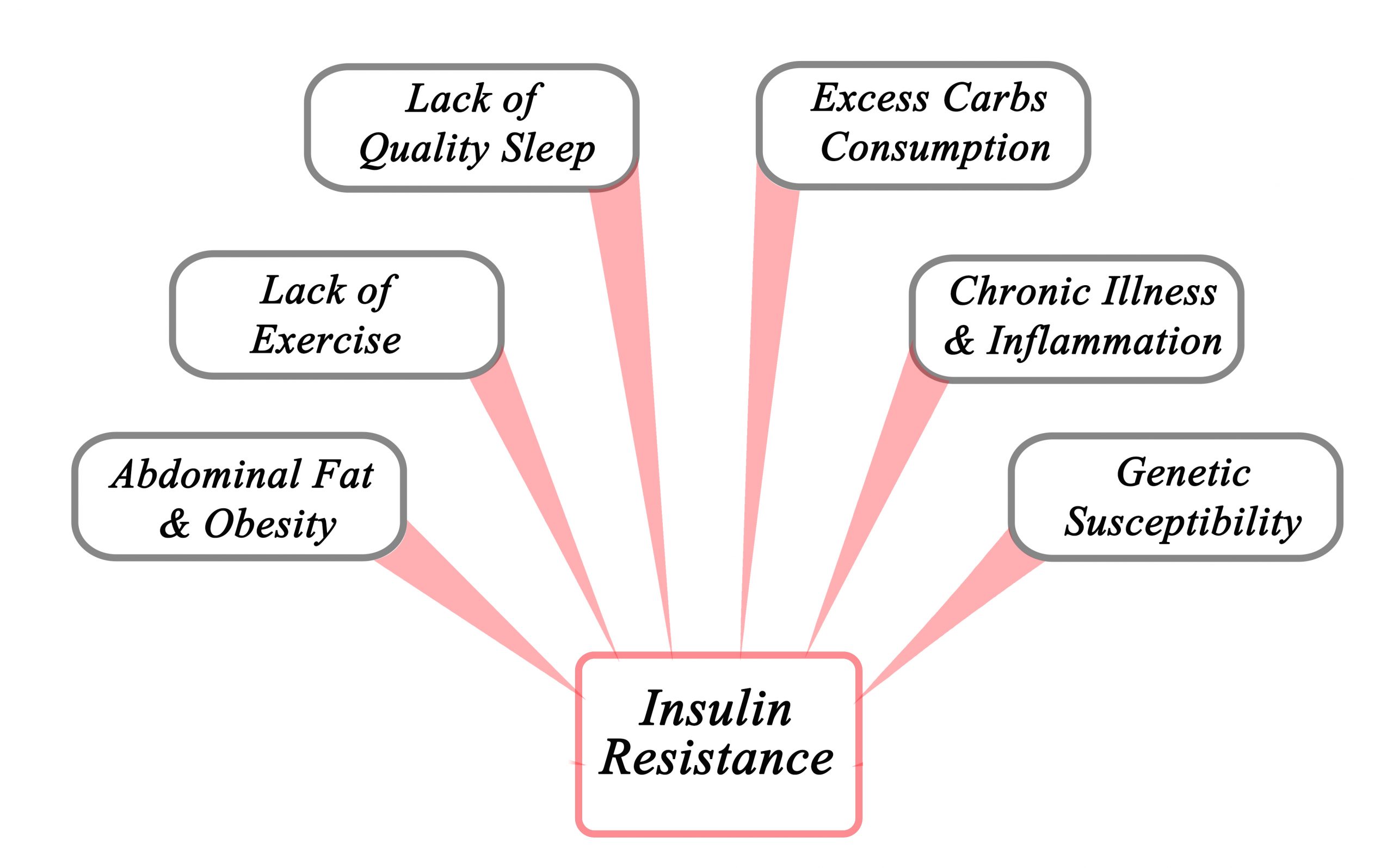
Insulin resistance can affect anyone, and it can be temporary especially if you are under stress or taking corticosteroid medication.
Other risk factors include: (taken from CDC website)
- overweight or obesity
- age 45 or older
- a parent, brother, or sister with diabetes
- African American, Alaska Native, American Indian, Asian American, Hispanic/Latino, Native Hawaiian, or Pacific Islander American ethnicity
- physical inactivity
- health conditions such as high blood pressure and abnormal cholesterol levels
- a history of gestational diabetes
- a history of heart disease or stroke
- polycystic ovary syndrome, also called PCOS
- certain medicines, such as glucocorticoids NIH external link, some antipsychotics, and some medicines for HIV
- hormonal disorders, such as Cushing’s syndrome and acromegaly
- sleep problems, especially sleep apnea
How to reverse insulin resistance
Check with your care provider before starting any lifestyle or dietary changes
- Increase physical activity- any activity that gets heart rate up increases insulin sensitivity.
- Consider intermittent fasting– In conjunction with a healthy diet, stress reduction, and physical activity, intermittent fasting has proven to increase insulin sensitivity and regulate glucose metabolism
- Lower carbohydrate intake- Talk with your care provider or a dietician about ways to lower carbohydrate intake. Work with them to put together a workable, realistic meal plan
- Reduce stress-In addition to avoiding stressful situations, and media that may prove upsetting try deep breathing exercises– proven to reduce stress and anxiety.
- Get good quality sleep- Practice sleep hygiene– shut off blue light emitting screens, turn off wifi (known to decrease melatonin production and increase norepinephrine- the fight or flight hormone- production)
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
FAQ: Our most commonly asked questions about Jase
Medical Readiness: What Really Kills First
When Disaster Strikes, It’s Not Hunger or Thirst That Takes the First Lives In every disaster zone, from hurricanes in the Caribbean to war zones in Ukraine, the pattern is the same. People worry about food and water, but it’s infection that kills first. A small wound...
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole *Disclaimer: This article is for educational purposes and does not constitute medical advice. Always seek professional guidance.* In the evolving...