3 Reasons EVERYONE should have emergency medications avaiable. It's all about access—access to medications and care when you need it most. And when things happen outside of your control that access can disappear.Below are 3 examples of how easily this access can be...
Antibiotic Resistance in the Clouds?


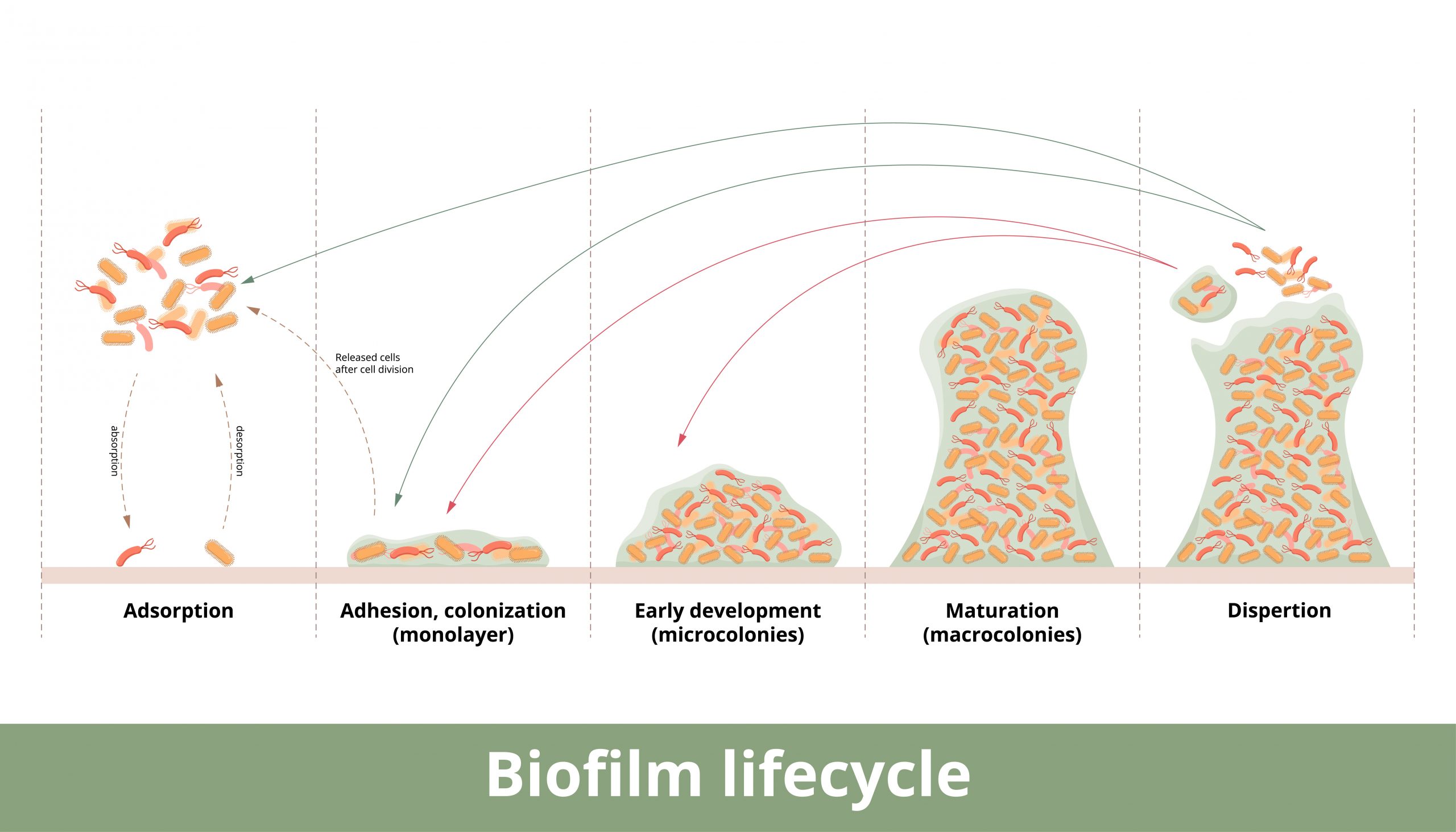
French and Canadian researchers discovered antibiotic resistant bacteria in clouds according to last month’s edition of the journal Science of The Total Environment. Between September 2019 and October 2021 high-flow rate impingers (vacuums) were deployed at the meteorological station of the puy de Dôme summit (elevation 4,806 ft)where they collected samplings of twelve clouds and analyzed total airborne bacterial concentration. What they found out was concerning. 29 antibiotic resistance genes were discovered over marine and continental environments. Analysis of the bacteria revealed an average of 8,000 bacteria per milliliter of cloud water. In addition, the clouds contained, on average, 20,800 copies of antibiotic-resistance genes per milliliter of cloud water. The bacteria analyzed are a normal part of the environment and are found on plants and in soil. The bacteria are picked up by wind or human activity and are carried up to the atmosphere and distributed throughout the clouds, and disseminated back to the environment.
Between 5 and 50 percent of these bacteria could be alive and active, according to researchers.
“This is the first study to show that clouds harbor antibiotic resistance genes of bacterial origin in concentrations comparable to other natural environments,” says Florent Rossi, first author of the study and postdoctoral fellow in the team of Caroline Duchaine, a professor at Université Laval’s Faculty of Science and Engineering and a researcher at the Quebec Heart and Lung Institute-Université Laval.
Widespread use of antibiotics in medicine and farm animals is speculated to contribute to the proliferation of these antibiotic resistant genes. Further research is needed to understand the health implications of this discovery.
Bacteria resistant genes discovered in the cloud samples
Bacteria resistant genes discovered in clouds and antibiotic examples
- Quinolone- ciprofloxacin, ofloxacin, enoxacin, perfloxacin, moxifloxacin and levofloxacin
- Sulfonamide- Bactrim, Bactrim DS, Septra, Septra DS.
- Tetracycline- lymecycline, methacycline, minocycline, rolitetracycline, and doxycycline
- Glycopeptide- vancomycin, teicoplanin, and ramoplanin
- Aminoglycoside- gentamicin, tobramycin, amikacin, plazomicin, streptomycin, neomycin, and paromomycin
- B-lactamase- oxacillin (IV), nafcillin (IV), dicloxacillin (PO)]
- Macrolide- Azithromycin, clarithromycin, and erythromycin
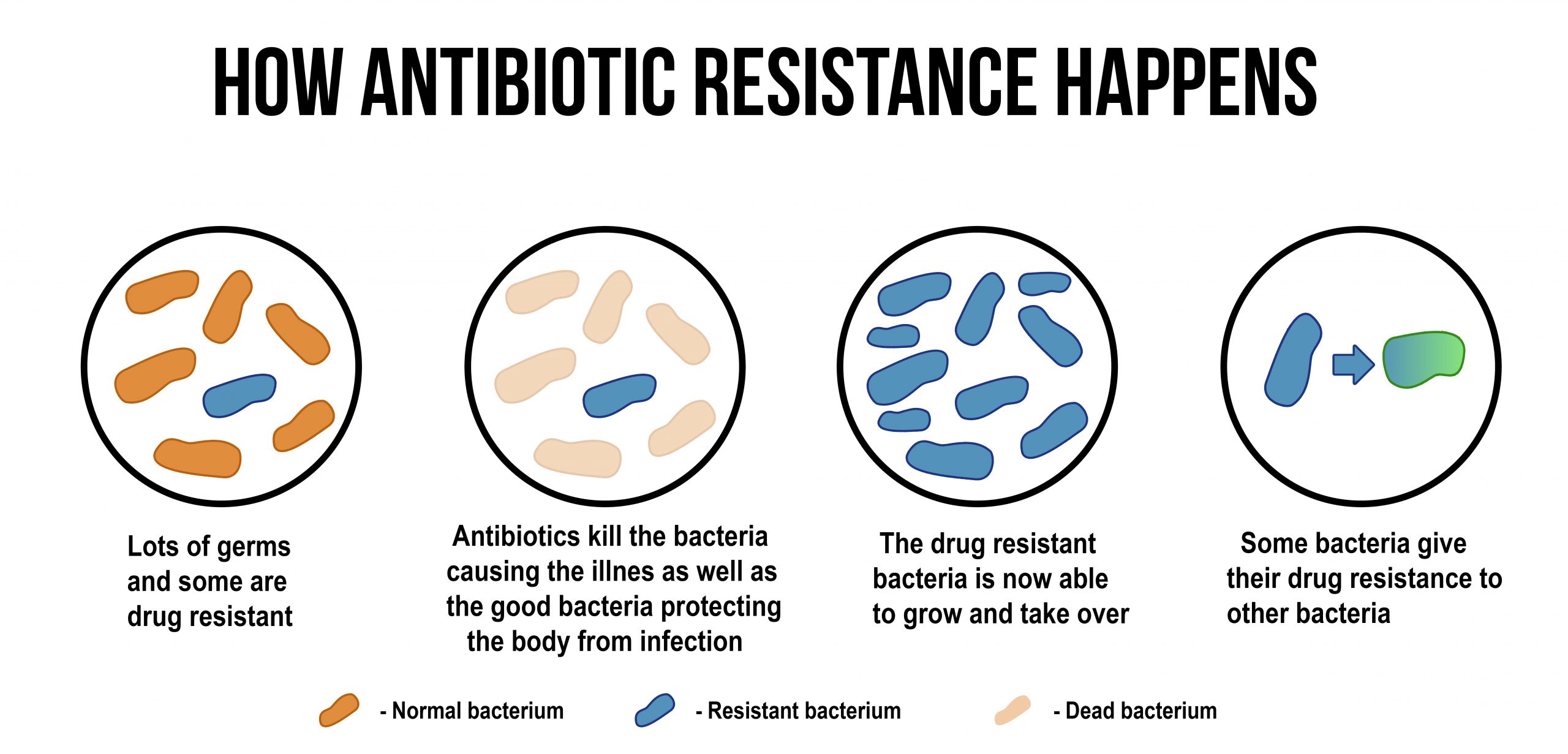
How widespread is antibiotic resistance?
Antimicrobial resistance is an urgent global public health threat, killing at least 1.27 million people worldwide and associated with nearly 5 million deaths in 2019. In the U.S., more than 2.8 million antimicrobial-resistant infections occur each year. More than 35,000 people die as a result, according to CDC’s 2019 Antibiotic Resistance (AR) Threats Report.
If antibiotics lose their effectiveness the ability to treat infections is lost.
How to fight antibiotic resistance
Antibiotic resistance spreads in a variety of settings. From hospitals (nosocomial infections) to everyday life, veterinary use of antibiotics, antibiotics in the food supply (poultry, beef, etc) and now, as demonstrated, by soil and water through clouds.
- Personal hygiene- wash hands after using bathroom and before eating or preparing food. After using bathroom, preparing food or coming home from being in public, immediately wash hands to prevent spread of infectious agents that you may have picked up while out of the house. Wash hands for at least 20-30 seconds.
- Brush teeth after eating. Streptococcus mutans, a common bacteria found in the mouth, is the main cause of tooth decay. Tooth decay can lead to infections throughout the body.
- Practice safe sex. Antibiotic resistance to gonorrhea according to the CDC now needs to be treated with two antibiotics at the same time. In addition, there is evidence that chlamydia and syphilis are developing antibiotic resistance.
- Keep your immune system in top shape. Reduce or eliminate sugar from your diet, exercise daily, reduce stress. Stress makes you more susceptible to infection. Quality sleep also promotes health.
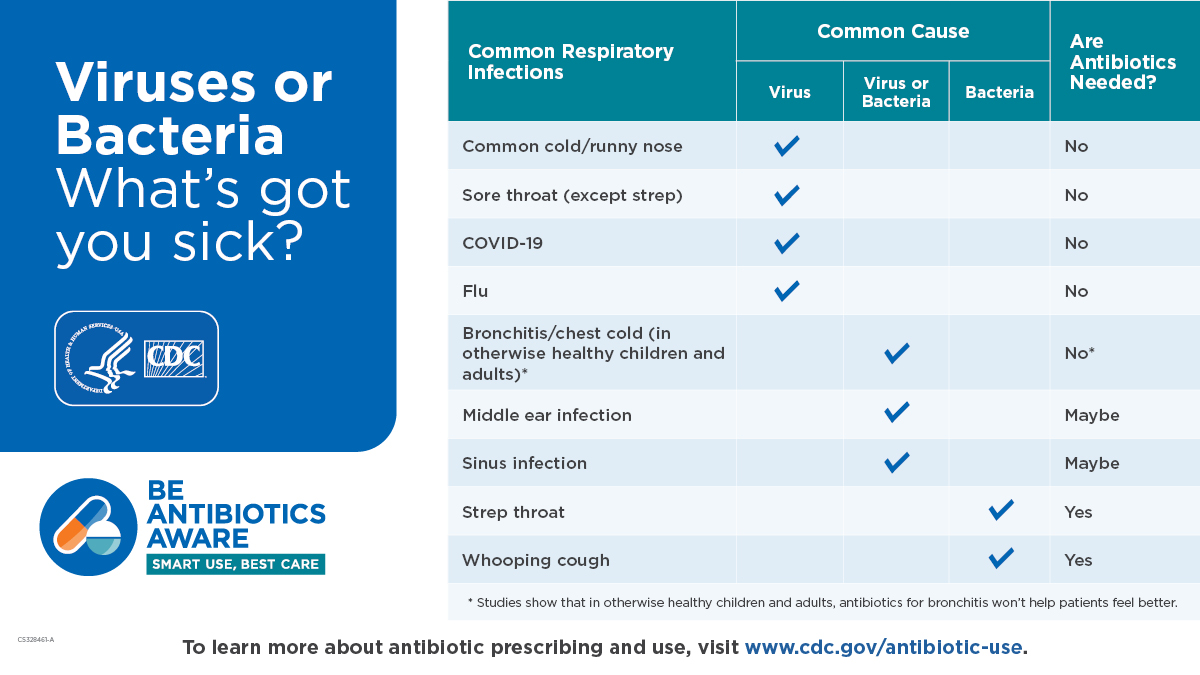
- Antibiotics kill bacteria and some fungal infections. They are ineffective with viral infections. Only use when needed.
- Finish the complete course of prescribed antibiotic unless otherwise instructed by your care provider. Use only when needed don’t “save” meds for another round of illness. This practice can cause antibiotic resistance.
- Avoid/sparingly use antibacterial hand sanitizers. These products have been found to cause antibiotic resistance.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
Be Prepared for Life’s Unexpected Moments
Youth Preparedness: Teaching, Building, and Coping with Disasters
Educating and preparing your children ahead of time means fewer surprises in the event of an emergency.Growing Up Prepared: Empowering Youth in Disaster Preparedness As we observe National Preparedness Month, it's crucial to remember that disasters can strike at any...
Low-Cost and No-Cost Emergency Preparedness Measures
Small steps today, mean a safer tomorrow for you and your loved ones.Low-Cost and No-Cost Emergency Preparedness So far in our series for National Preparedness Month this September, we've already covered How to Make an Emergency Plan for Your Household and How to...