Part 1 will cover
- Hashimoto’s description
- Prevalence of Hashimoto’s
- Symptoms of low thyroid (Is it Hashimotos?)
- Other not as common hypothyroid conditions
- Lab tests to diagnose Hashimoto’s
- Medications to treat low thyroid/Hashimotos
Part 2 will cover:
Tips to manage Hashimoto’s along with medications such as
- Health risks of not treating Hashimoto’s adequately
- Lifestyle/stress reduction tips to manage energy and emotional ups and downs
- How to naturally increase biologically active T3
- Diet strategies to help heal
- Nutritional supplements that can aid in recovery and optimal health
- How to advocate for yourself in the healthcare field when dealing with Hashimoto’s
Description
Hashimoto’s thyroiditis is an autoimmune disease that affects the thyroid. An autoimmune disease is a condition in which the body’s immune system mistakes its own healthy tissues as foreign and attacks them. Most autoimmune diseases cause inflammation of the affected tissue. In the case of Hashimoto’s thyroiditis, the thyroid gland is inflamed and attacked by the body’s immune system.
Note: any word with “itis” at the end indicates inflammation. (Arthritis, bursitis, conjunctivitis for example)
Over 90% of hypothyroid cases are Hashimoto’s.
Other causes of low thyroid are:
(Excerpt from American Thyroid Association)
- Pituitary gland disorder/damage-The pituitary, the “master gland,” tells the thyroid how much hormone to make. When the pituitary is damaged by a tumor, radiation, or surgery, it may no longer be able to give the thyroid instructions, and the thyroid may stop making enough hormone.
- Medicines-Medicines such as amiodarone, lithium, interferon alpha, and interleukin-2 can prevent the thyroid gland from being able to make hormone normally. These drugs are most likely to trigger hypothyroidism in patients who have a genetic tendency to autoimmune thyroid disease.
- Too much or too little iodine. The thyroid gland must have iodine to make thyroid hormone. Iodine comes into the body in food and travels through the blood to the thyroid. Keeping thyroid hormone production in balance requires the right amount of iodine. Taking in too much iodine can cause or worsen hypothyroidism.
- Surgical removal of part or all of the thyroid gland due to nodules or cancer
- Radiation treatment-Patients with Hodgkin’s disease, lymphoma, or cancers of the head or neck are treated with radiation. All these patients can lose part or all of their thyroid function.
- Congenital hypothyroidism (hypothyroidism that a baby is born with). A few babies are born without a thyroid or with only a partly formed one. A few have part or all their thyroid in the wrong place (ectopic thyroid). In some babies, the thyroid cells or their enzymes don’t work right.
- Rare disorders that infiltrate the thyroid. In a few people, diseases deposit abnormal substances in the thyroid and impair its ability to function. For example, amyloidosis can deposit amyloid protein, sarcoidosis can deposit granulomas, and hemochromatosis can deposit iron.
Prevalence of Hashimoto’s
- Most common in women– The American Thyroid Association (ATA) estimates that five to eight women are affected with Hashimoto’s for every one man. The ATA also estimates that one in eight women will be affected with Hashimoto’s or another thyroid disorder at some point in their lives.
- Runs in families (genetic predisposition)
- Affects about 5 percent of the US population
- It is suspected that it is underdiagnosed
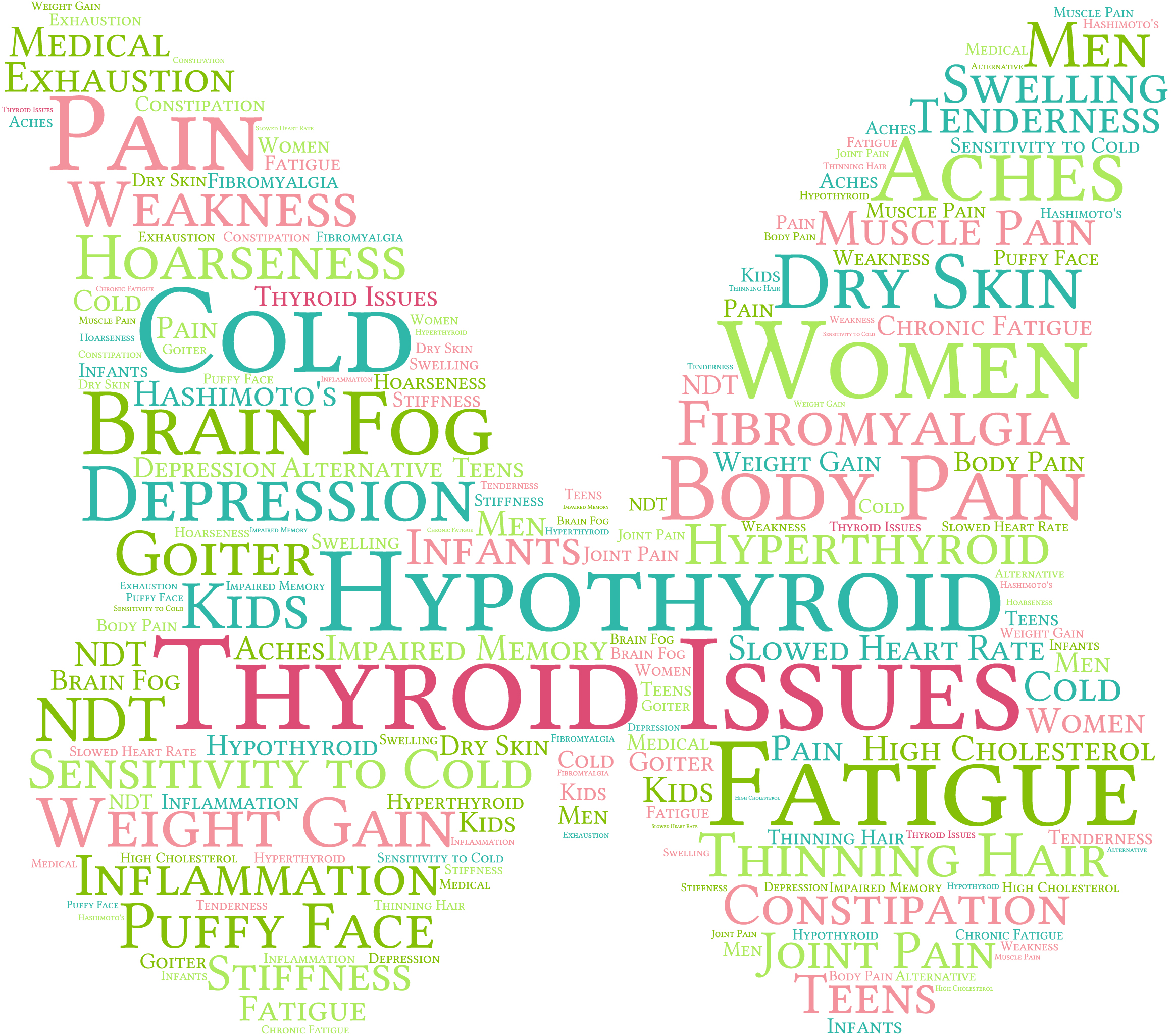
Symptoms
The onset of Hashimoto’s disease can be difficult to diagnose. As thyroid hormones are released in the bloodstream from antibodies attacking the thyroid, transitory (temporary)hyperthyroidism (high thyroid) results.
Early symptoms can mimic hyperthyroid. This condition presents as an elevated T3 (the biologically active form of thyroid) and elevated T4, along with suppressed TSH. This condition is called thyrotoxicosis (Hashitoxicosis). This phase can last for 1-2 months, however in rare cases this phase can last for 2 or more years.
Early-temporary symptoms can include
- Anxiety
- Nervousness
- Diarrhea
- Sleeplessness
- Mood swings and muscle weakness.
As the disease progresses (the autoimmune attack continues) thyroid production decreases, resulting in hypothyroidism (Hashimoto’s thyroiditis).
Symptoms of low thyroid are:
- Dry skin,
- Hair loss,
- Constipation,
- Depression,
- Intolerance to cold,
- Low energy
- Brain fog,
- Heavy menstruation,
- Unexplained weight gain.
- Muscle aches and cramps
Your care provider will take a thorough physical history (which includes checking for enlarged thyroid gland) and medical history along with a family history and your symptoms.
Lab tests for Hashimoto’s
TSH – The pituitary gland produces this hormone which stimulates the thyroid gland to produce thyroid hormone
Free T4– Free T4 is thyroid hormone not bound to protein, it is freely flowing in bloodstream.
Thyroid peroxidase antibodies (TPOAb) – Thyroid peroxidase (TPO) antibodies are a type of thyroid antibody. Thyroid peroxidase is an enzyme which helps to make thyroid hormones (T3, T4 and TSH). The body’s immune system makes antibodies in response to non-self proteins. These non-self proteins are called antigens.
Thyroglobulin antibodies (TGAb) – Thyroglobulin antibodies (Tg Ab) are another type of thyroid antibody. Thyroglobulin is a protein made by thyroid cells. It helps to make thyroid hormones. Thyroglobulin antibodies (Tg Ab) are made when the body attacks it’s own thyroglobulin. Thyroglobulin antibodies can be raised in Hashimoto’s thyroiditis They are also raised in 10-15% of the general population.
You may be diagnosed with Hashimoto’s disease if your TSH is high, your free T4 is low, and your TPO Ab is elevated. High TPO Ab is the key marker because it is present in over 90% of those with Hashimoto’s. TG Ab is present in about 60-80% of cases.
- Low T3 levels may mean you have hypothyroidism,
- T3 test results are often compared with T4 and TSH test results to help diagnose thyroid disease.
Reverse T3-as symptoms dictate
Reverse T3 is created by the body from T4. Your body can convert T4 into the ACTIVE thyroid hormone T3 or the inactive thyroid called reverse T3. Reverse T3 slows metabolism to conserve energy during times of extreme stress and inflammation.
Treatment
Hashimoto’s requires a multi prong approach. Along with medication, and lifestyle/stress management, diet and supplements can go a long way to achieve optimum health. Diet, lifestyle and supplements will be covered in part 2.
Medications
Note: A word about generic and label medications- Though the names are different, generic and brand-name drugs work the same. According to the FDA, generic drugs are just as effective as their branded counterparts. Drug makers must prove that generic medications can be substituted for brand-name drugs and offer the same benefits as their brand-name counterparts
Levothyroxine – also known as Synthroid Euthyrox, Unithroid, Tirosint. and Levoxyl– These medications use only T4 hormone as primary ingredient.
One advantage to generic levothyroxine, unlike Synthroid is it does not contain corn. This is invaluable for anyone with an allergy or sensitivity to corn.
Armour thyroid- Desiccated thyroid- made from bovine thyroid hormone- contains both T4 and T3
Cytomel – (generic name is liothyronine) – A manmade T3 hormone
There are many other brands of thyroid medications, however the above represents the majority of medications.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
FAQ: Our most commonly asked questions about Jase
If you’re considering Jase, chances are you’ve paused and thought, “This makes sense, but I still have a few questions.”You’re not alone. Here are the most common ones we hear, answered plainly. Is this really doctor-prescribed? Yes. Every Jase order is reviewed by a...
Medical Readiness: What Really Kills First
When Disaster Strikes, It’s Not Hunger or Thirst That Takes the First Lives In every disaster zone, from hurricanes in the Caribbean to war zones in Ukraine, the pattern is the same. People worry about food and water, but it’s infection that kills first. A small wound...
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole *Disclaimer: This article is for educational purposes and does not constitute medical advice. Always seek professional guidance.* In the evolving...