When Disaster Strikes, It’s Not Hunger or Thirst That Takes the First Lives In every disaster zone, from hurricanes in the Caribbean to war zones in Ukraine, the pattern is the same. People worry about food and water, but it’s infection that kills first. A small wound...
Does Your Sore Throat Need an Antibiotic?

Antibiotics don’t kill viruses; they kill bacteria, mold, or parasites.
They are lifesaving drugs when the need arises. However, overuse has led to antibiotic-resistant strains of bacteria that used to be effective with an appropriate antibiotic. Nowadays, we are facing a crisis of antibiotic resistance, leading many healthcare providers to use caution when prescribing antibiotics.
Some bacteria and mold have mutated and developed immunity to common antibiotics, leaving healthcare providers with fewer options. However, with judicious use, there are still several effective antibiotics available. Knowing when to use them and when to treat symptoms is essential.
This is especially true when dealing with a sore throat. While nothing can replace a healthcare provider visit and lab testing, some telltale signs can help determine if you need an antibiotic to treat your sore throat.
There may be a time soon, given all the worldwide unrest you won’t be able to visit your healthcare provider- staff shortage, cyber-attacks on their laboratory and computer systems, medical supply shortage (throat swabs, etc.).
Example of a viral infection leading to a bacterial infection
A viral infection can weaken the immune system and allow pathogenic, opportunistic bacteria to grow. This is called a secondary or coinfection infection. For example, a case of influenza (viral) can lead to mycoplasma pneumonia (bacterial) or even strep throat.
How can you tell the difference if you are without medical care? If medical systems and testing are not available, you must rely on exposure, symptoms, and susceptibility to infection to guide you.
To begin with, let’s look at the difference between a bacterial, fungal, and viral infection.
Bacterial Infection
Bacteria are single-cell organisms that can live in diverse (many different) environments- in soil, air, almost anywhere. (see below) Most are not disease-causing.
Disease-causing bacteria are called pathogenic bacteria. Pathogenic bacteria invade and reside in the host (human or animal) and can cause illness.
Common bacterial infections include:
- Strep throat (causes sore throat)
- Cellulitis (commonly caused by group B strep)
- Lyme disease (transmitted via tick bite)
- Urinary tract infections
- Bacterial meningitis (caused by Streptococcus pneumoniae, Group B Streptococcus, Neisseria meningitis, Haemophilus influenzae, Listeria monocytogenes, Escherichia coli)
- Staphylococcus aureus – the most common form of healthcare facility-related infections
Less common but a public health threat is Mycobacterium tuberculosis (tuberculosis or TB).
Fungal Infection
Fungus are eukaryotic (with a nucleus) organisms that are either single cells, such as yeast, or molds, which are a collection of cells that form long, thin, hairlike threads called hyphae. Just like bacterial infections, they can live almost anywhere: air, surfaces, etc.(see below)
Symptoms of strep throat
(need antibiotics)
- Fever
- Pain when swallowing
- Sore throat that can start very quickly and may look red
- Red and swollen tonsils
- White patches or streaks of pus on the tonsils
- Tiny, red spots on the roof of the mouth, called petechiae
- Swollen lymph nodes in the front of the neck
- Strep throat can lead to rheumatic fever
Note: It is crucial to take an entire course of antibiotics, stay home from work or school until you no longer have a fever, AND have taken antibiotics for at least 12 hours.
The following symptoms suggest a virus is causing the illness instead of strep throat:
- Cough
- Runny nose
- Hoarseness (changes in your voice that make it sound breathy, raspy, or strained)
- Conjunctivitis (also called pink eye)
If a virus is the cause of a sore throat, antibiotics will not help.
(need antibiotics)
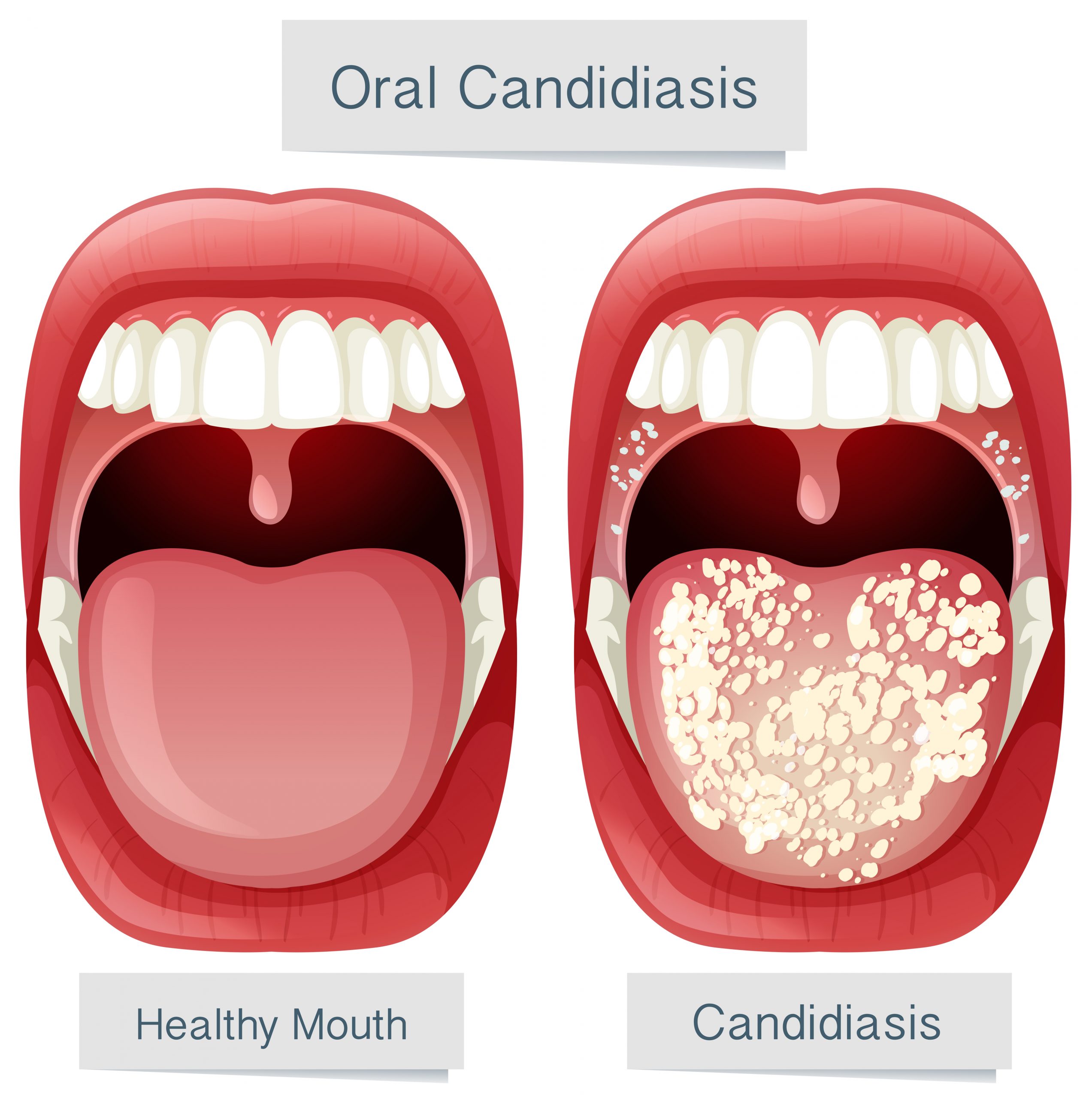
Candidiasis is an infection caused by a yeast (a type of fungus) called Candida. Candida usually lives on the skin and inside the body, in places such as the mouth, throat, gut, and vagina, without causing any problems. Candida can multiply and cause an infection if the environment inside the mouth, throat, or esophagus changes in a way that encourages fungal growth.
Candidiasis in the mouth and throat:
- White patches on the inner cheeks, tongue, roof of the mouth, and throat
- Redness or soreness
- Pain while eating or swallowing
- Cracking and redness at the corners of the mouth
You are at risk for developing Candida if you:
- Wear dentures
- Have diabetes
- Have cancer
- Have HIV/AIDS
- Take antibiotics or corticosteroids, including inhaled corticosteroids
- Take medications that cause dry mouth
- Smoke
Treatment
Candidiasis in the mouth, throat, or esophagus is treated with antifungal medicine. The treatment for mild to moderate infections in the mouth or throat is usually an antifungal medicine applied to the inside of the mouth for 7 to 14 days. These medications include clotrimazole, miconazole, or nystatin. The most common treatment for severe infections is fluconazole (an antifungal medication) taken by mouth or vein.

- Candidiasis- throat, mouth (causes sore throat)
- Candidiasis-vaginal can lead to urinary tract infection
- Nail fungus
- Ringworm
- Aspergillosis
- Blastomycosis
- Candida Aureus (C.aureus)
Viral Infection
Viruses are tiny (much smaller than bacteria) parasitic microorganisms that feed off living cells or tissue in the body. Viruses can quickly spread from one person to another through the same routes as bacteria and fungi. (see below)
Common viral infections include:
- Influenza (can cause sore throat)
- Common cold (can cause sore throat)
- Covid 19 (can cause sore throat)
- RSV (respiratory syncytial virus) (can cause sore throat)
- Hepatitis
- Viral pneumonia (can impair the immune system, leading to bacterial infection)
- Viral meningitis
- Chickenpox
How bacteria, mold, and viruses are transmitted (how they infect the body)
- Droplets or aerosol (cough or sneeze)
- Body fluids (infected wound -bacterial or sexual contact- both bacterial and viral)
- Tick bites
- Bug bites
- Contact with contaminated surfaces (faucets, sharing utensils or cups, towels or personal items)
- Eating or drinking contaminated food or water
- Dust or decaying matter
- Nosocomial (hospital origin)
A robust immune system can prevent bacterial, fungal, and viral infections. Susceptible people are those being treated for cancer, the very young, the elderly, diabetics, and anyone with impaired immune function.
How to tell if your sore throat needs an antibiotic.
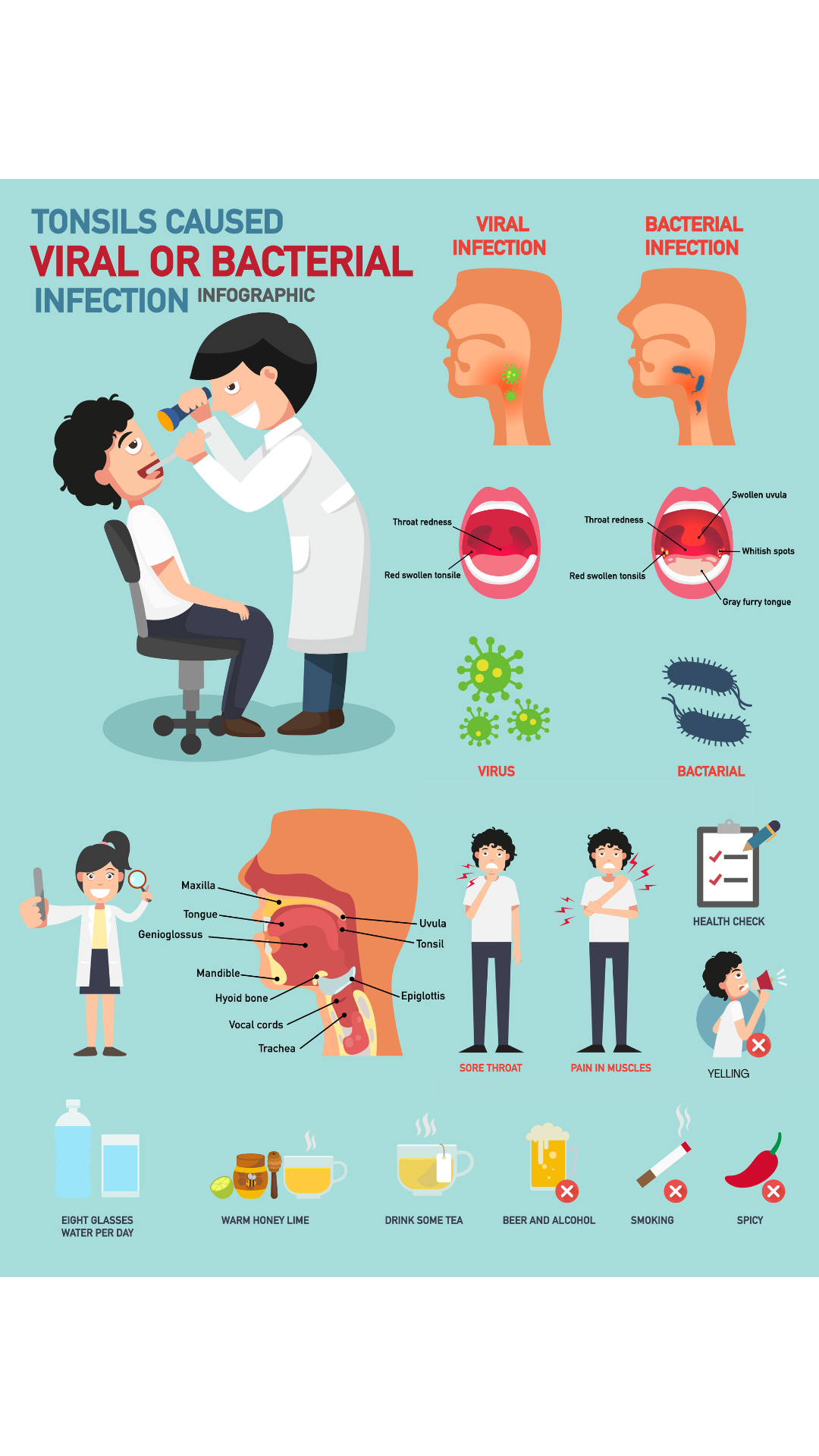
Most sore throats are caused by a virus, such as a cold or flu, and do not require an antibiotic—other common causes of a sore throat- strep throat and oral candidiasis (thrush), require antibiotics.
Symptoms and Treatment of Sore Throats
The following is only a guideline in the event there is no medical care available. In addition, consult your healthcare provider for guidance and advice.
According to the CDC, most sore throats, except strep throat and candidiasis, do not need antibiotics.
Sore throat pain relief
- Suck on ice chips, popsicles, or lozenges (do not give lozenges to children younger than 4 years).
- Use a clean humidifier or cool mist vaporizer.
- Gargle with salt water.
- Drink warm beverages and plenty of fluids.
- Use honey to relieve cough for adults and children at least 1 year or older.
- Over-the-counter symptom and pain relievers.
Warm/hot water with honey, ginger, and lemon drink can reduce phlegm and soothe the throat lining. In addition, ginger has proven antibacterial, antiviral, and anti-inflammatory properties.

The Jase Case with add-ons have you covered, with antibiotics and pain relievers for sore throats and many other types of infections.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
Medical Readiness: What Really Kills First
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole *Disclaimer: This article is for educational purposes and does not constitute medical advice. Always seek professional guidance.* In the evolving...
Be Prepared for Life’s Unexpected Moments
3 Reasons EVERYONE should have emergency medications avaiable. It's all about access—access to medications and care when you need it most. And when things happen outside of your control that access can disappear.Below are 3 examples of how easily this access can be...
Youth Preparedness: Teaching, Building, and Coping with Disasters
Educating and preparing your children ahead of time means fewer surprises in the event of an emergency.Growing Up Prepared: Empowering Youth in Disaster Preparedness As we observe National Preparedness Month, it's crucial to remember that disasters can strike at any...