If you’re considering Jase, chances are you’ve paused and thought, “This makes sense, but I still have a few questions.”You’re not alone. Here are the most common ones we hear, answered plainly. Is this really doctor-prescribed? Yes. Every Jase order is reviewed by a...
How Long Do My Meds Last? A Look at Ciprofloxacin
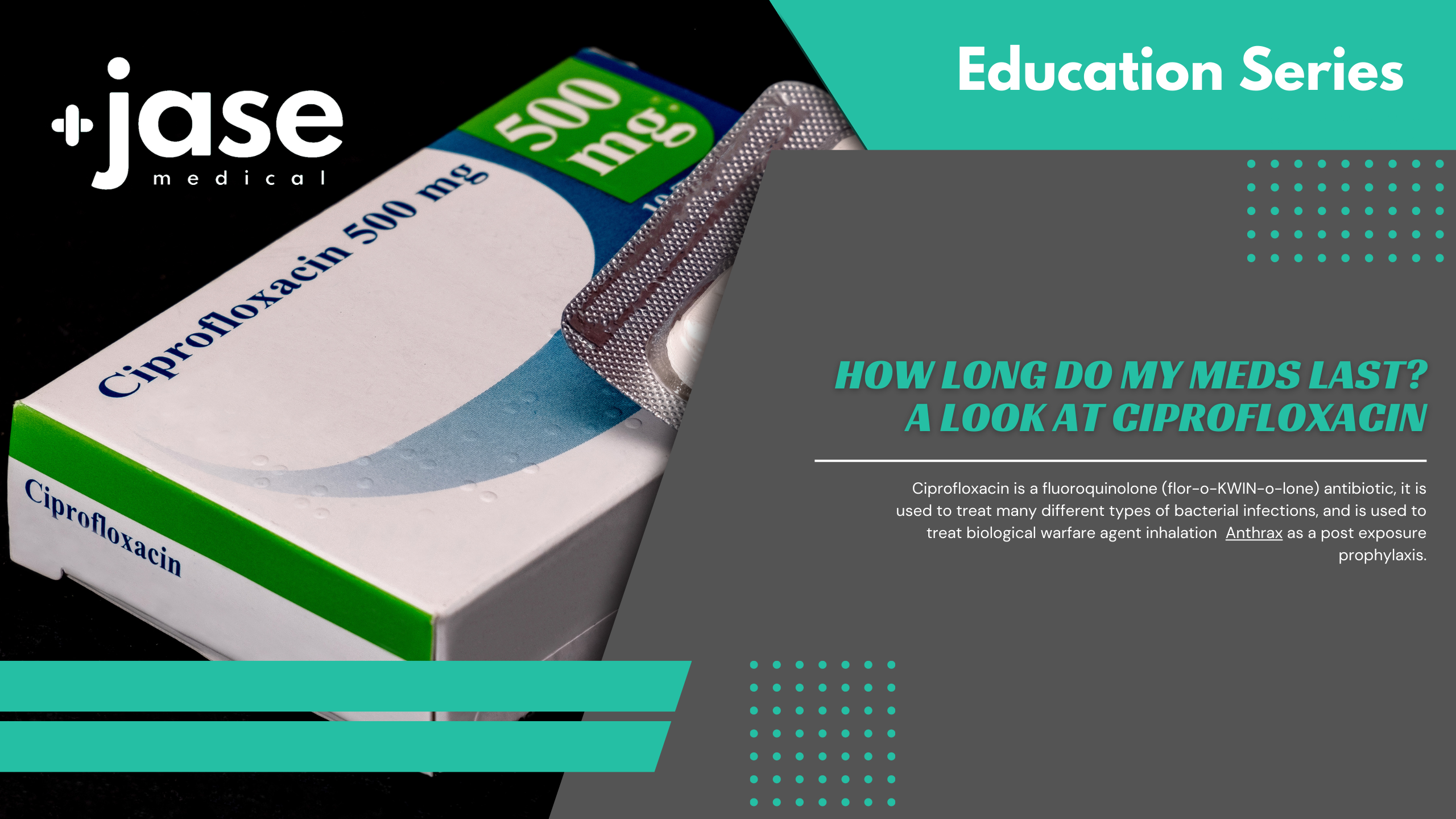
(How about over 10 years past expiration?)

Ciprofloxacin is a fluoroquinolone (flor-o-KWIN-o-lone) antibiotic, it is used to treat many different types of bacterial infections, and is used to treat biological warfare agent inhalation Anthrax as a post exposure prophylaxis.
How long does ciprofloxacin remain potent?
When stored in a cool, dry, and dark area away from sunlight and capped, ciprofloxacin can retain much of its potency well past expiration date.
Expiration dates reflect the time during which the product is expected to remain stable, or retain its identity, strength, quality, and purity, when it is properly stored according to its labeled storage conditions. According to the Shelf-Life Extension Program, a joint initiative of the FDA and Department of Defense that tested 122 drugs for potency after their expiration date revealed ciprofloxacin maintained its active ingredients with no deterioration in strength for up to 142 months- over 10 years!
Ciprofloxacin is listed in the World Health Organization Model List of Medications for the newly released 2023 edition:
FIRST CHOICE (From WHO 2023 list)
- Acute invasive bacterial diarrhea /dysentery
- Enteric fever
- Low-risk febrile neutropenia
- Pyelonephritis or prostatitis (mild to moderate)
SECOND CHOICE (From WHO 2023 list)
- Cholera
- Complicated intraabdominal infections (mild to moderate)
In addition, ciprofloxacin can be used to treat:
- Anthrax exposure
- Tularemia
- Urinary tract infection
How to Take
Take ciprofloxacin dose 2 hours before or 6 hours after taking other medicines. It may be taken with or without food. Drink plenty of liquids when taking ciprofloxacin.
Side Effects
Fluoroquinolones carry black box warning
Fluoroquinolones (FQ) have been associated with increased tendon ruptures. A tendon rupture is a partial or complete tear of a tendon.
A large study reviewing retroactive patient records was conducted between 2007 and 2016 with over a million subjects from the senior population age 65 and older. This study reviewed the use of FQ against other antibiotics and even similar drugs in the FQ class to assess tendon rupture occurrence. Only one of the FQ antibiotics displayed a significant tendency to tendon rupture- between a 16% (rotator cuff) and fourfold risk (Achilles tendon). That antibiotic was levofloxacin. Neither ciprofloxacin-one of the antibiotics found in the Jase case- or moxifloxacin- which were part of the study- was found to increase tendon rupture.
For more information, please read this post: Does Ciprofloxacin (Cipro) cause tendon rupture?
What To Avoid
- Do not take ciprofloxacin with dairy products such as milk or yogurt, or with calcium-fortified juice.
- Avoid antacids that contain calcium, magnesium, or aluminum (such as Maalox, Milk of Magnesia, Mylanta, Pepcid Complete, Rolaids, Tums, and others).
- Vitamin or mineral supplements that contain calcium, iron, magnesium, or zinc.
- Ciprofloxacin can cause sun sensitivity. Avoid sunlight or tanning beds. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
Consult with your care provider before taking if you are taking any of the following:
-
- Oral diabetes medicine
- Products that contain caffeine
- Medicine to treat depression or mental illness
- Steroid medicine (such as prednisone)
- NSAIDs (nonsteroidal anti-inflammatory drugs) – aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve), celecoxib, diclofenac,
- Clozapine, cyclosporine, methotrexate, phenytoin, probenecid, ropinirole, sildenafil, or theophylline
- A blood thinner (warfarin, Coumadin, Jantoven)
- Heart medication or a diuretic indomethacin, etc.
For a more complete list of drugs that may interact with ciprofloxacin check out this site.
Make your care provider aware if you currently have (or history of)
- Low levels of potassium in blood
- Muscle weakness, myasthenia gravis
- Any history of heart disease
- Aneurysm
- Diabetes or low blood sugar
- You or family history of long QT syndrome
- Brain tumor, head injury or seizures
- Liver or kidney disease
- Nerve problems
- If pregnant or breastfeeding consult your primary care provider for guidance. There is evidence that ciprofloxacin can affect the fetus and enter breast milk. Ciprofloxacin carries US FDA pregnancy category C (Animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks).
Common ciprofloxacin side effects may include:
- Nausea, vomiting, diarrhea, stomach pain
- Headache
- Abnormal liver function tests
Seek medical attention if you experience:
- Signs of an allergic reaction to ciprofloxacin (hives, difficult breathing, swelling in your face or throat) or a severe skin reaction
- Low blood sugar – hunger, irritability, nausea, fast heart rate, or feeling shaky
- Nerve damage symptoms – numbness, crawling, pins and needles or tingling, burning pain in your hands, arms, legs, or feet
- Serious mood or behavior changes – nervousness, agitation, hallucinations, memory problems, thoughts of suicide
- Bloody or black, tarry stools
Discontinue and seek immediate medical attention if you experience:
- Severe pain in your chest, stomach, or back (a rare but serious side effect of ciprofloxacin) which may damage the aorta, leading to bleeding or death
- Fast or pounding heartbeats, fluttering in your chest, shortness of breath, and sudden dizziness (like you might pass out)
- Muscle weakness
- Breathing problems
- Little or no urination
- Jaundice (yellowing of the skin or eyes)
- Increased pressure inside the skull – severe headaches, ringing in your ears, vision problems, pain behind your eyes.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
FAQ: Our most commonly asked questions about Jase
Medical Readiness: What Really Kills First
When Disaster Strikes, It’s Not Hunger or Thirst That Takes the First Lives In every disaster zone, from hurricanes in the Caribbean to war zones in Ukraine, the pattern is the same. People worry about food and water, but it’s infection that kills first. A small wound...
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole
Exploring Dr. William Makis’ Hybrid Orthomolecular Cancer Protocol: Focus on Ivermectin and Mebendazole/Fenbendazole *Disclaimer: This article is for educational purposes and does not constitute medical advice. Always seek professional guidance.* In the evolving...