Pneumonia is an infection of the tiny air sacs of the lung called alveoli. Alveoli absorb oxygen from inhaled air. When alveoli become infected, they fill up with fluid, making transport of oxygen throughout the body difficult. Pneumonia can range in severity from a mild illness to a severe, even life-threatening illness.
2.56 million people died from pneumonia in 2017. Almost a third of all victims were children younger than 5 years, it is the leading cause of death for children under 5. (after premature birth)
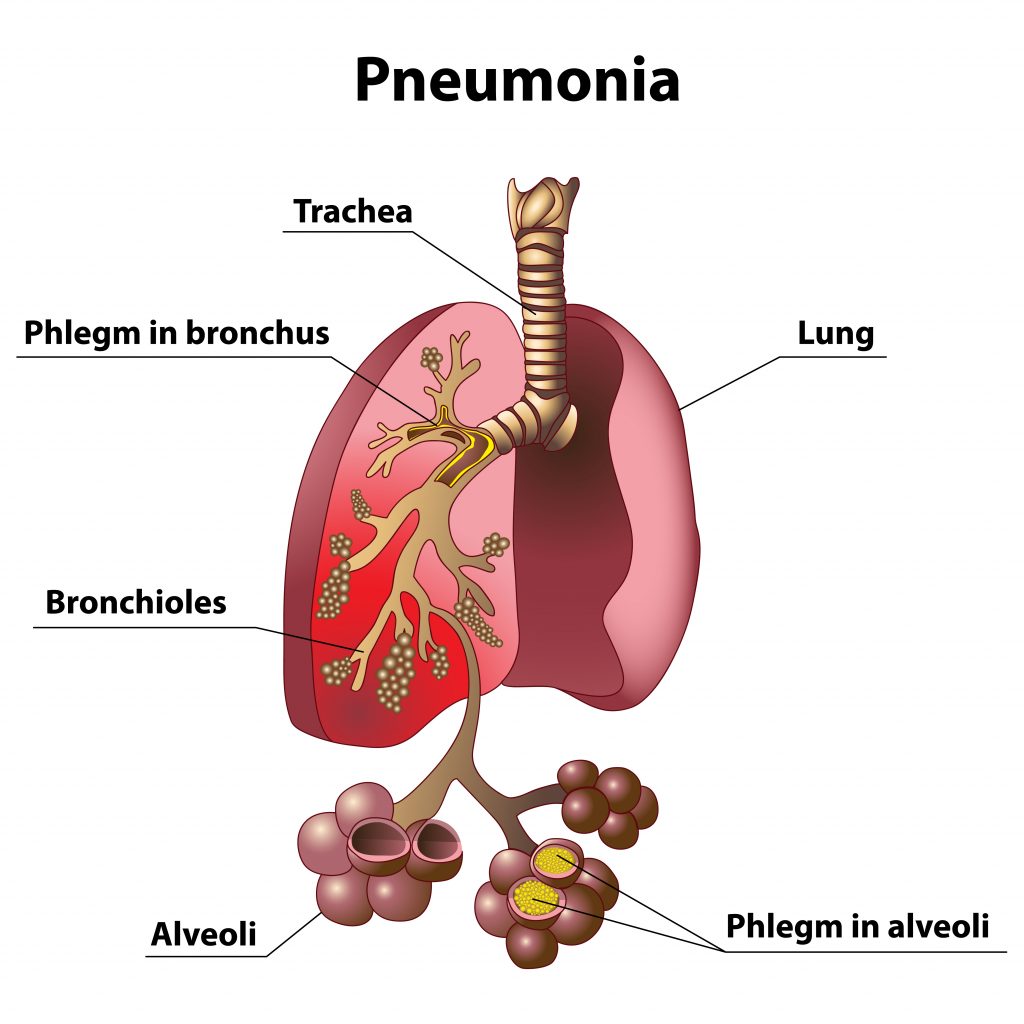
Phlegm in the lungs during pneumonia
Who gets pneumonia?
Pneumonia is a very common illness, which any person can develop. People more likely to get pneumonia include adults 65 years or older, children younger than 5 years old, people who smoke, people with ongoing health conditions, such as chronic obstructive pulmonary disease (COPD), diabetes, congestive heart failure, sickle cell anemia, or conditions that weaken the immune system, such as HIV/AIDS, cancer therapy, or organ transplantation. Pneumonia might also be more likely to occur after some kinds of lung injury – for example, after lungs have been damaged from breathing in chemicals.
How is pneumonia spread?
Some germs that cause pneumonia can spread through the air, by direct contact with an infected person, or by contact with contaminated objects. Some causes of pneumonia can come from the environment and can be spread in dust or other fine particles (e.g., water vapor). Some germs that cause pneumonia are not spread from person to person – for example, a person who loses control of breathing (e.g., during a seizure or while intoxicated) could vomit and then inhale stomach contents and bacteria into the lungs and develop pneumonia.
There are 3 types of pneumonia. Bacterial, viral and fungal pneumonia.
Bacterial pneumonia. Pneumococcal disease is caused by bacteria called Streptococcus pneumoniae and is the most common type of bacterial pneumonia. Other bacterial causes of pneumonia are Haemophilus influenzae, Mycoplasma pneumoniae Staphylococcus aureus (commonly found in healthcare settings), Chlamydia, Legionella species. Bacterial pneumonia is treated with antibiotic therapy. A vaccine is available for some strains of bacterial pneumonia.
Pneumococcus bacteria can cause infections in many parts of the body, including
- Lungs (pneumonia)
- Ears (otitis)
- Sinuses (sinusitis)
- Brain and spinal cord tissue (meningitis)
- Blood (bacteremia)
Complications of pneumococcal pneumonia include:
- Infection of the space between membranes that surround the lungs and chest cavity (empyema)
- Inflammation of the sac surrounding the heart (pericarditis)
- Blockage of the airway that allows air into the lungs (endobronchial obstruction), with collapse within the lungs (atelectasis) and collection of pus (abscess) in the lungs.
- Walking pneumonia- Mycoplasma pneumoniae bacteria commonly cause mild infections of the respiratory system. The most common illness caused by these bacteria, especially in children, is tracheobronchitis (chest cold). Lung infections caused by M. pneumoniae are sometimes referred to as “walking pneumonia” since symptoms are generally mild. Sometimes M. pneumoniae can cause more serious lung infections that require care in a hospital.
Viral pneumonia cannot be treated with antibiotics. Antivirals are sometimes prescribed, along with symptom management. Common causes of viral pneumonia are influenza, respiratory syncytial virus (RSV), and SARS-CoV-2 (the virus that causes COVID-19).
NOTE: Secondary infection of bacterial pneumonia can happen after a person becomes ill with influenza or another virus. At that point, an antibiotic would be indicated.
Fungal pneumonia is caused by the inhalation of spores and is difficult to diagnose. It is estimated that up to 20% of people infected are unaware they have it. It can sit latent for years, and sometimes resolve itself on its own. It is treated with antifungal medication.
The signs and symptoms of pneumonia
- Cough, which may produce greenish, yellow, or even bloody mucus
- Fever, sweating, and shaking chills
- Shortness of breath
- Rapid, shallow breathing
- Sharp or stabbing chest pain that gets worse when you breathe deeply or cough
- Loss of appetite, low energy, and fatigue
- Nausea and vomiting, especially in small children
- Confusion, especially in older people
When to call the doctor
If pneumonia is suspected due to symptoms and the patient is under the age of 5 or immune-compromised or has other risk factors such as heart or lung disease, smokers, asthmatics, and diabetics call healthcare provider. Early detection can lead to reduced hospital stays can be lifesaving.
Call your healthcare provider for the following symptoms if the above risk factors don’t apply:
- Bluish tinge to lips, fingers
- Difficulty in taking deep breaths
- Chest congestion which is painful when breathing
- Consistent fever of 102 or above degrees Fahrenheit
- A hacking cough which produces phlegm or pus
- A fever that resolves then comes back after a few days. This can be an indicator that a viral illness has a secondary bacterial pneumonia in addition to the virus.
How are different types of pneumonia classified?
The various types of pneumonia are classified according to a number of characteristics. To treat these types, it’s essential to know whether somebody caught pneumonia at home, in a hospital, or in a nursing home.
Community-acquired and nosocomial pneumonia
If you develop pneumonia at home, it’s referred to as community-acquired pneumonia (or CAP for short), even if you are admitted to the hospital during the course of the illness.
If you develop pneumonia while in the hospital, it is called hospital-acquired (HAP for short) or nosocomial pneumonia. Pneumonia is considered to be nosocomial if it starts at least two days after you are admitted to the hospital, or within three months of a hospital stay.
Doctors can also classify pneumonia even more exactly, considering whether somebody became infected in a retirement or a nursing home, at a medical facility such as a dialysis center, or while receiving artificial respiration.
Why is classification important for the treatment?
Community-acquired pneumonia is usually caused by pneumococci, whereas nosocomial pneumonia is often connected with staphylococci, various intestinal bacteria, and special germs such as Pseudomonas aeruginosa. Some of those bacteria can be multi-resistant, meaning they are resistant to several antibiotics. That is why different antibiotics are usually needed then for treating community-acquired pneumonia.
Mild, moderate or severe pneumonia
To be able to provide the right treatment, doctors also classify community-acquired pneumonia as mild, moderate, or severe.
Pneumonia is considered to be mild with no increased risk if the patient is:
- is younger than 65 years old,
- is conscious and lucid,
- has normal blood pressure and pulse,
- is not breathing too fast (fewer than 30 breaths per minute),
- has enough oxygen in their blood,
- has not been given any antibiotics in the past three months,
- has not been in the hospital in the past three months, and
- does not have any other severe medical conditions.
People with mild pneumonia can be treated at home and are given antibiotics or antivirals in tablet form.
Symptomatic treatments for mild pneumonia include:
- Over the counter pain reliever reducers such as Tylenol, Advil or Aleve (Note: do not give aspirin to young children)
- Expectorants to help thin out secretions and bring up phlegm
- Avoid smoke and secondhand smoke
- Use a humidifier
- Steamy baths help open airways
- Warm fluids, keep hydrated to thin secretions and bring up phlegm
Avoid cough suppressants unless recommended by your healthcare provider.
The signs of moderate pneumonia include drowsiness and confusion, low blood pressure, worsening shortness of breath, and risk factors such as old age and underlying diseases. People with these symptoms need to have treatment at a hospital. Some will be given a combination of two different antibiotics, at least at the beginning of the treatment.
Pneumonia is classified as severe when the heart, the kidneys or the circulatory system are at risk of failing, or if the lungs can no longer take in enough oxygen. Treatment with an antibiotic infusion in intensive care is then usually needed, sometimes with artificial respiration or additional drugs such as corticosteroids.
Pneumonia in children is only classified as either “not severe” or “severe.”
There seems to be confusion about the color of phlegm/sputum and what it means as far as the infection is concerned. Yellow or green phlegm or sputum can be indicative of an infection. However, viral bronchitis presents as green sputum as a normal feature as does bacterial load from those with COPD. Given the rising incidence of antibiotic resistance sputum or phlegm color should only be one of other symptoms associated with the initiation of antibiotic therapy.
How can pneumonia be prevented?
- Avoid close contact with people who are sick
- Stay home from work or school when you are sick
- Cover your mouth and nose when coughing or sneezing
- Wash your hands often with soap and water. (or use an alcohol based hand sanitizer if soap and water are not available)
- Avoid touching your eyes, nose or mouth
- Get vaccinated against germs that cause respiratory illness (influenza, pneumococcus, etc)
- There are several versions of pneumococcal conjugate vaccine (PCV) which target different serotypes of S. pneumoniae-the bacterium responsible for most cases of pneumonia
- Avoid air pollution and other respiratory irritants such as tobacco products and secondhand smoke
- Promote breastfeeding According to Laura Lamberti et al. (2013), pneumonia mortality of children in developing countries who are not breastfed in the first 5 months of their lives is 15 times greater than those who exclusively received their mother’s milk.
- Get adequate nutrition and rest
How long can an infected person carry the germs that cause pneumonia?
Most people who are exposed to the germs that cause pneumonia do not become ill or develop only mild respiratory illness. Fewer develop pneumonia. How long a person can spread a respiratory germ depends on the type of germ and the treatment the person receives (antibiotic therapy, etc.) For some cases of pneumonia, such as influenza or tuberculosis individuals need to stay home until they are no longer contagious. Consult your primary health provider for guidance in these instances.
