As 2022 marches on, our world is becoming increasing unstable. Worldwide conflicts are causing worldwide, nationwide, and local problems.
We are now faced with out-of-control gas prices, which will have a trickle-down effect, not just at the gas pump, but in every part of our economy and lives. Trucks may soon not find it profitable to deliver food, materials, and even medical supplies. Store shelves, which are already showing signs of shortages and escalating food prices may soon be at a point where the food may be in stock but unaffordable.
Inflation just hit a 4 decade high and there is no end in sight.
 Add to this state and federal agencies warn healthcare providers of imminent cyberattacks.
Add to this state and federal agencies warn healthcare providers of imminent cyberattacks.
“The Cybersecurity and Infrastructure Security Agency (CISA), the Federal Bureau of Investigation (FBI), and the Department of Health and Human Services (HHS). Issued an advisory that cybercriminals were planning on targeting healthcare systems with ransomware for financial gain.”
As I have pointed out in previous articles China and India play an integral part in our medication production and raw materials to make medications. With world events affecting these supply chains we really could be looking at a catastrophe in the making.
Cognitive dissonance-the mental conflict that occurs when beliefs or assumptions are contradicted by new information.
For many, the belief and wish is that our lives will go back to “normal”. This is highly unlikely, and in order to survive and thrive in this “new normal” we must learn to adapt to our every changing situations.
Our mind is our greatest asset- or liability
Resilience and adaptability
“Psychologists define resilience as the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress—such as family and relationship problems, serious health problems, or workplace and financial stressors. As much as resilience involves “bouncing back” from these difficult experiences, it can also involve profound personal growth.”
Over the past two years many have been able to find equilibrium, balance, and ability to cope. Others did not. Alcohol abuse rose during the pandemic. Suicide was at an all-time high for our youth.
In order to survive and thrive in this new world we need to either have or develop skills that can help us cope. Don’t feel you need to go it alone. There is help. Our mindset is everything in this new world we are seeing unfold. If you or a loved one needs help Mentalhealth.gov has resources to help you or your loved one cope and develop resiliency skills.
Our mind as our friend or foe will make or break us.
Act, don’t react
- Coping with the vast changes around us requires a different way of life, in our interpersonal relationships, how we work, play, eat and travel. We can see the glass as half full or half empty. Develop an attitude of gratitude. It really is up to us. Stay calm, and keep a rational mindset, don’t panic.
- Take, for example, the out-of-control gas prices. For some it is necessary to commute, given the fact that work and daycare are on opposite parts of town. Perhaps your employer would allow you to work a 4 days a week schedule, and either work longer hours or take some work home? That would save on time, gas, and maybe even daycare.
If you are on a bus line, many buses are now equipped with front bike racks. Taking advantage of these racks could offer you a light workout.
Facing out of control grocery bills? Community gardens are a great way to lower your food budget, grow vegies, connect with community, and learn different gardening skills. Contact your local city hall for a list of community gardens in your area.
In addition, microbes in soil are powerful antidepressants. Gardening provides not only food for the body, but food for the soul.
If you are living in and apartment or have limited space, there are some wonderful you tube videos on container and indoor gardening.
- Cyberattacks on our grid and computers are something out of our control, but with a preparedness mindset we can mitigate and not allow these situations to affect us as much as they would otherwise.
- Check your water supply-Cyberattacks can affect infrastructure such as utilities and water supplies.
- Plan on at least 5 gallons of water a day per person. You should have on hand least 2 weeks’ worth of clean, purified water, or a way to purify water. (See previous articles for guidance)
- Food– are you stocked up and do you have easy to prepare food (and can opener)? Do you have way to heat food? Menu planning and utilizing your local USDA ag extension will help keep your grocery costs down and in case of grid down situation you will be equipped to handle this.
- Have activities for all members of the family in case the electric grid and internet goes down. Taking up a hobby such as reading, drawing, string arts, musical instruments.
- Medical supplies, medications, and supplements. Make sure you have ample supply to get you through the most challenging and extended crisis. Talk to your healthcare provider about having extra medications on hand in case of supply disruption.
We will get through this, focus on what you can do and not what you can’t. Even though our way of life is rapidly changing, we can see it as an opportunity for growth.

As the pandemic winds down, more countries are opening their borders to international visitors. The postponed trips to see loved ones, business trips, tourism and medical tourism are slowly becoming a reality. Given a little forethought and planning will make your travel plans go smoothly.
We will cover the following:
- The everchanging landscape of mandates, quarantines, isolation, and vaccinations for each country, can cause confusion surrounding rules and regulations with each country. Do you need to be vaccinated against covid or will a negative covid test do? Quarantine?
- What are recommended medications to bring while traveling?
- How do I travel with medications, especially prescription medication?
- How do I locate medical attention and medication if there is a medical emergency while out of the states?
Covid travel and restrictions
Due to the evolving nature and rules surrounding these questions the CDC travel destinations page has an alphabetical list of countries and their restrictions regarding covid 19 and immunizations. As your planned trip get closer, please check back with this site as the rules frequently change.
When traveling abroad, you are exposed to different germs, time zones, food, and water. A little planning and equipped with the right medications will help make your trip enjoyable and keep you out of a health clinic or hospital in a land where it may be difficult or near impossible to source healthcare.

Medications to Have While Traveling
Note: Many nonprescription medications have interactions and can be dangerous if taken by individuals with prescribed medications or health conditions. As with all medications consult your primary care provider. Follow the hyperlink (to Drugs.com) associated with each medication listed for more information.
Note: As with all drugs, if pregnant, nursing or using with small child always consult your primary care provider for guidance.
- Anti-diarrheal, such as Kaopectate or Pepto Bismol (bismuth subsalicylate) In case of mild diarrhea from contaminated food or water (also known as travelers’ diarrhea) or lack of hygienic practices this medicine is especially important. When traveling, you may not be able to easily locate restrooms. If you are between flights, or in a vehicle where no facilities are available for an extended period of time this medicine can prove to be invaluable. Be sure to stay hydrated while experiencing diarrhea symptoms. Other uses include upset stomach and nausea. If diarrhea continues past a few days or fever present, an antibiotic may be indicated. (See Jase case below)
Note– Do not use if bleeding ulcer, abdominal pain (other than mild cramping) or allergy to aspirin, or with small children. There are drug interactions, check with care provider before using. Do not use more than 2 days or when fever present.
- Laxative/stool softener-Colace 2-in-1 Docusate/senna When traveling across time zones, out of your regular routine, eating strange foods, and limiting liquids while on the road, constipation can strike. A mild laxative with stool softener can help alleviate these symptoms. Be sure to drink plenty of liquids when taking a laxative. Do not use if rectal bleeding or upset stomach are present. Do not take for longer than a week if no bowel movement after one day of use.
- Anti-nausea/motion sickness– Dramamine, (dimenhydrinate) Whether on a cruise, plane, train or traveling by car, motion sickness can ruin a much-anticipated trip. If you are prone to motion sickness, use 30-60 minutes before travel. This medication can cause sleepiness and reduced reflexes as a side effect. There are numerous side effects and interactions and cautions when using this medication. Kidney and liver disease, glaucoma, overactive thyroid, high blood pressure are just a few of the contraindications for use. Do not drive or operate machinery while using.
- Pain reliever, fever reducer, anti-inflammatory– Tylenol (acetaminophen), Advil (ibuprofen) or Aleve (naproxen) Depending on preference- single dose packs of pain relievers. Discuss with your primary care provider which they recommend. Care must be taken with any pain reliever/ fever reducer/ anti-inflammatory. There are many health conditions and medication interactions that can dictate which pain reliever to take. Note: Tylenol is not anti-inflammatory. Advil and Aleve are. There are many differences between the different pain relievers. Tylenol is recommended to take every 4-6 hours (there is a timed release one that is taken every 8 hours), Advil every 6- 8 hours. Aleve is taken every 12 hours, which may be more convenient when traveling, however it is not recommended for small children.
- Antihistamine Benadryl (diphenhydramine) Benadryl has many uses. As an antihistamine it works to help relieve allergic symptoms such as water eyes, sneezing and runny nose. It is also useful as an anti-nausea medication and is used extensively in nursing homes as a sleep aid. Benadryl can cause drowsiness and should not be taken with alcohol. Young children should not take unless recommended by their care provider.
- Jase Case The 5 prescription antibiotics found in this pack can treat many illnesses encountered by travelers. From urinary tract infections to infectious diarrhea to infected wounds to pneumonia and more, this pack of antibiotics can prove indispensable and bring peace of mind. Medical care may be difficult to locate, sourcing the correct medicine to treat symptoms could be even harder. As a prescription medication, travel between countries becomes much easier. The booklet provided covers a wide array of health conditions which will guide you as to whether to take an antibiotic and which one to take if needed.
- Prescription medications and supplements– Make sure your medications are properly labeled and stored correctly. Traveling out of country can present challenges. Be sure to have plenty of medications on hand (at least a week or more) in case of travel delays.
More information when traveling with prescription medications and supplements:
(Taken from the CDC website on travel)
- Make an appointment with a travel medicine specialist or your health care provider to get needed vaccines and medicines at least 4 to 6 weeks before you leave.
- If you plan to be gone for more than 30 days, talk to your doctor about how you can get enough medicine for your trip. Sometimes insurance companies will pay for only a 30-day supply at a time.
- Ask your doctor about any changes to taking your medicine once you’re in a different time zone. Medicines should be taken according to the time since your last dose, not the local time of day.
- Ask how to safely store medicine and check whether it needs refrigeration. Keep in mind that extreme temperatures can reduce the effectiveness of many medicines.
- Pack smart and put your medicines and supplements in your carry-on luggage. You don’t want to be stuck without them if your suitcase gets lost!
- Bring enough medicine to last your whole trip, plus a little extra in case of delays.
- Keep medicines in their original, labeled containers. Ensure that they are clearly labeled with your full passport name, doctor’s name, generic and brand name, and exact dosage.
- Bring copies of all prescriptions, including the generic names for medicines.
- Leave a copy of your prescriptions at home with a friend or relative in case you lose your copy or need an emergency refill.
- Pack a note on letterhead stationery from the prescribing doctor (preferably translated into the language understood at your destination) for controlled substances, such as marijuana, and injectable medicines, such as EpiPens and insulin.
- Check with the foreign embassy of the country you will be visiting or passing through to make sure your medicines are permitted in that country.
-
- Be aware that many countries only allow taking a 30-day supply of certain medicines and require the traveler to carry a prescription or a medical certificate.
- If your medicine is banned at your destination, talk with your health care provider about alternative medicine or destination options, and have your doctor write a letter describing your condition and the treatment plan.
- The International Narcotics Control Board (INCB) provides general information about country regulations for travelers carrying medicines that are made with controlled substances. It’s important to note that INCB may not have information from all countries or territories.
If you must buy drugs during your trip in an emergency, there are ways to reduce your chances of buying counterfeit drugs:
- Contact the nearest US embassy or consulate. They should be able to connect you with doctors and pharmacies that can help you find reliable, quality medicines.
- Buy medicines only from licensed pharmacies and get a receipt. Do not buy medicines from open markets.
- Ask the pharmacist whether the drug has the same active ingredient as the one you were taking.
- Make sure the medicine is in its original packaging.
- Look closely at the packaging. Sometimes poor-quality printing or otherwise strange-looking packaging will indicate a counterfeit product.
A few additional items when traveling
- Water purification tablets these tablets take a few hours to work when added to water but are effective in purifying water polluted with chemicals and bacteria.
- Small bandages for minor cuts and blisters
- Small set tweezers and scissors (may need to check these with luggage)
- Moleskin for prevention and pain relief from shoe friction
- A few packets of oral rehydration solution powder
- Lifestraw water bottle with filter– filters bacteria and chemical pollutants, and are handy when enroute to destination
- Small pack of hand wipes for times when facilities with water and soap are unavailable
- Small packs triple antibiotic ointment
- Small penlight with batteries
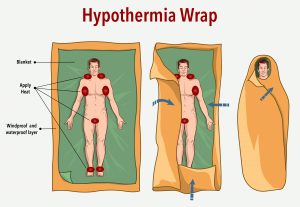
What is hypothermia?
- Hypothermia is caused by prolonged exposures to cold temperatures. When exposed to cold temperatures, your body begins to lose heat faster than it’s produced. Lengthy exposures will eventually use up your body’s stored energy, which leads to lower body temperature. Cold temperatures can be brought on by a number of factors such as ambient air, dampness, water, and wind exposure to name a few.
- Body temperature that is too low affects the brain, making the victim unable to think clearly or move well. This makes hypothermia especially dangerous, because a person may not know that it’s happening and won’t be able to do anything about it.
- While hypothermia is most likely at very cold temperatures, it can occur even at cool temperatures (above 40°F) if a person becomes chilled from rain, sweat, or submersion in cold water. Heat loss to air and water are the most common causes of hypothermia.
In fact, most cases of hypothermia occur when temperatures are between 30 and 50 degrees F. Windy conditions and wet clothes can work together to chill the unaware, even on a summer day. In water temperatures from 70-80 degrees, exhaustion or unconsciousness can set in within 3-12 hours; 60-70 degrees, 2-7 hours, and in water from 50-60 degrees, you could be unconscious in 1-2 hours.
Statistics
Each year there are approximately 700 to 1500 patients in the United States who have hypothermia noted on their death certificate. Adults between the ages of 30 to 49 are more likely affected, with men being ten times more likely than women. However, the true incidence of hypothermia is relatively unknown. Even with supportive in-hospital care, the mortality of those with moderate to severe hypothermia still approaches 50 percent.
Who’s most at risk?
Victims of hypothermia are often:
- Older adults
- Babies sleeping in cold bedrooms
- Small children due to the lower body mass
- People who remain outdoors for long periods—the homeless, hikers, hunters, boaters, people who work outdoors in the elements, etc.
- People who drink alcohol or use illicit drugs.
- In addition to hypothermia from environmental exposure, many medical conditions can cause hypothermia including hypothyroidism, adrenal insufficiency, sepsis, neuromuscular disease, malnutrition, thiamine deficiency, and hypoglycemia (low blood sugar)
- The most common medications that put one at risk for hypothermia are antianxiety drugs, antidepressants, antipsychotics, and opioids.
Symptoms of hypothermia
Adults and children:
- Shivering (in the beginning shivering may be a sign of hypothermia, however it isn’t always present).
- Exhaustion or feeling very tired
- Confusion
- Fumbling hands
- Memory loss
- Slurred speech
- Drowsiness
Babies:
- bright red, cold skin
- very low energy
Hypothermia is a medical emergency. If you notice any of the above signs, take the person’s temperature. If it is below 95° F, get medical attention immediately!
If you are not able to get medical help right away, try to warm the person up.
- Get the person into a warm room or shelter.
- Remove any wet clothing the person is wearing.
- Warm drinks can help increase body temperature, but do not give alcoholic drinks. Do not try to give beverages to an unconscious person.
- Warm the center of the person’s body—chest, neck, head, and groin—using an electric blanket, if available. You can also use skin-to-skin contact under loose, dry layers of blankets, clothing, towels, or sheets.
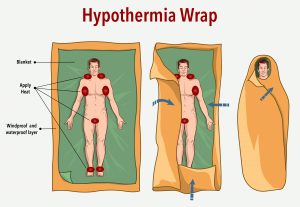
- Get the person proper medical attention as soon as possible.
A person with severe hypothermia may be unconscious and may not seem to have a pulse or to be breathing. In this case, handle the person gently, and get emergency assistance immediately.
- Perform CPR, even if the person appears dead. CPR should continue until the person responds or medical aid becomes available. Keep warming the person while performing CPR. In some cases, hypothermia victims who appear to be dead can be successfully resuscitated.
How to prevent hypothermia
- Dress in loose layers, allowing air trapped between clothing to maintain warmth
- Make sure you are hydrated.
- Eat sufficient calories to maintain body heat
- If caught in an emergency situation don’t eat snow, it will drop your core body temperature. Only drink water or other liquids that are above freezing point
- Small children (and elderly) may not be aware they are cold, always be aware of their clothing- hat, gloves, boots, dry warm socks are essential wear
Frostbite
What is frostbite?
Frostbite is a type of injury to the skin caused by freezing. It leads to a loss of feeling and color in the areas it affects, usually extremities such as the nose, ears, cheeks, chin, fingers, and toes. Frostbite can permanently damage the body, and severe cases can lead to amputation (removing the affected body part).
Who’s most at risk?
Those at risk for frost bite:
- Have poor blood circulation
- Are working outside in the cold
- Are not properly dressed for extremely cold temperatures
- Are exposed to a cold wind chill
- People who have cardiac insufficiency, diabetes and stroke
- Heavy alcohol consumption
What are the signs and symptoms of frostbite?

If you notice redness or pain in any skin area, get out of the cold or protect any exposed skin—frostbite may be beginning. Any of the following signs may point to frostbite:
- A white or grayish-yellow skin area
- Skin that feels unusually firm or waxy
- Numbness to exposed area. Ears, nose, chin, hands, and feet are most at risk for frostbite
A person who has frostbite may not know they have it until someone else points it out because the frozen parts of their body are numb.
If you notice signs of frostbite on yourself or someone else, seek medical care. Check to see if the person is also showing signs of hypothermia. Hypothermia is a more serious condition and requires emergency medical care.
If (1) a person shows signs of frostbite, but no signs of hypothermia and (2) immediate medical care is not available, do the following:
- Get the person into a warm room as soon as possible.
- Unless absolutely necessary, do not walk on feet or toes that show signs of frostbite—this increases the damage.
- Do not rub the frostbitten area or massage it at all. This can cause more damage.
- Put the areas affected by frostbite in warm—not hot—water (the temperature should be comfortable to the touch for unaffected parts of the body).
- If warm water is not available, warm the affected area using body heat. For example, you can use the heat of an armpit to warm frostbitten fingers.
- Do not use a heating pad, heat lamp, or the heat of a stove, fireplace, or radiator for warming. Affected areas are numb and can easily burn.
Don’t substitute these steps for proper medical care. Frostbite should be checked by a health care provider.
The following is an excerpt from the American Association of Dermatology:.
How to prevent frostbite
- Dress in loose, light, comfortable layers. Wearing loose, light layers helps trap warm air. The first layer should be made of a synthetic material, which wicks moisture away from your body. The next layer should be insulating. Wool and fleece are good insulators and hold in more body heat than cotton. The top layer should be windproof and waterproof. A down parka and ski pants can help keep you dry and warm during outdoor activities.
- Protect your feet and toes. To protect your feet and toes, wear two pairs of socks. The first pair, next to your skin, should be made of moisture-wicking fabric. Place a pair of wool or wool-blend socks on top of those. Your boots should also provide adequate insulation. They should be waterproof and cover your ankles. Make sure that nothing feels tight, as tight clothing increases the risk of frostbite.
- Protect your head. To protect your ears and head, wear a heavy wool or fleece hat. If you are outside on a bitterly cold day, cover your face with a scarf or face mask. This warms the air you breathe and helps prevent frostbite on your nose and face.
- Protect your hands. Wear insulated mittens or gloves to help protect your hands from the cold.
- Make sure snow cannot get inside of your boots or clothing. Wet clothing increases the risk of developing frostbite. Before heading outdoors, make sure that snow cannot easily get inside of your boots or clothing. While outdoors, if you start to sweat, cut back on your activity or unzip your jacket a bit.
- Keep yourself hydrated. Becoming dehydrated also increases the risk of developing frostbite. Even if you are not thirsty, drink at least one glass of water before you head outside, and always drink water or a sports drink before an outdoor workout. In addition, avoid alcohol, as it increases your risk for frostbite.
- Recognize the symptoms. In order to detect frostbite early, when it’s most treatable, it’s important to recognize the symptoms. The first signs of frostbite include redness and a stinging, burning, throbbing, or prickling sensation followed by numbness. If this occurs, head indoors immediately.
At 1PM Monday January 3rd, 2022, Senator Tim Kaine started his 2-hour commute from his Virginia home to Washington DC. This 2-hour commute turned into a 27-hour ordeal. A surprise blizzard, dumping about a foot of snow paralyzed both lanes of traffic on Interstate 55, causing hundreds of motorists to be stranded along one of the East Coasts busiest thoroughfares. Senator Kaine stated he had a warm coat and a full tank of gas. He also stated he hadn’t had anything to eat except an orange that a family coming back from Florida was handing out from the box of oranges that they had picked up while vacationing.
Senator Kaine was in a highly traveled route, one where you would not expect that traffic could be at a standstill for over 24 hours. Luckily, no one needed medical care during this ordeal. It could have turned out disastrous.

Moral of this story: A weather emergency can happen to anyone, anytime, anywhere.
Commuting, whether by car, bus, subway, train, or bike can have unexpected emergencies that can spell disaster for the unprepared.
Just because your travels take you through highly populated areas doesn’t make you immune to the perils of adverse weather events.
Winter travel can be life threatening, especially if you haven’t prepared.
In high rainfall areas flooding is common. Roads can be swept away from flood waters; rivers can overrun their banks. Mudslides can close roads. High winds can knock down power lines and tip over high sided vehicles. Fog limits visibility and can be treacherous. Avalanches are also a danger. While driving home 2 men were caught in an avalanche that buried their car. Luckily, they had cellphone service and were able to call for help.
Medical preparedness extends beyond what is in your medicine cabinet (which is important). In the case of cold weather, being prepared is essential.
At home you are in a much more stable environment compared to travel. Hopefully you have thought about what to do if your lights and source of heat are out for an extended time due to a weather event (ice storm, high winds, tornado, hurricane, etc.) If not, take a few minutes to note and make a list of what you may need. There are many lists and advice on the internet. So, I won’t go into too much detail. However, a home based medical supply list should include:
- Basic first aid kit
- Prescription medication and a way to prepare and take it
- Flashlights with extra batteries (Headlamps are handy, it frees hands for other chores, especially in a medical emergency)
- A safe way to stay warm (indoor safe propane heater, for instance)
- Backup power for anyone on oxygen or cpap or other medical devices.
Even a last-minute trip to the grocery store before a storm can prove life threatening.

If you must drive in this weather there are some apps you can download to your phone that could help you decide if, when and best route to take. These should only be used for areas with strong cell phone coverage. An essential item for anyone traveling in rural or spotty cellphone areas is the Garmin GPS. These devices were issued to staff at my place of employment when I worked in rural Idaho. These and devices like these are used by backwoods skiers, hikers, and rural workers. These devices use satellites and can send a SOS signal to whomever you set them up for, along with EMS services.
A few well thought out items can mean the difference between life and death when traveling. Not having a change of socks after stepping out of the vehicle to clear snow from the exhaust can lead to hypothermia. Know the signs of hypothermia and what to do.
Skipped medications can also be life threatening.
Action Plan:
Inventory your car, take note of what you have and what you need to get prepared. If your main source of travel is subway or bus, dedicate a small backpack to items necessary to wait out an emergency if transportation comes to a halt for an extended period of time.
Some travel items to include would be:
Note- if traveling on public transportation you won’t be able to carry all items listed, nor will you need to. A small pack with extra meds, drinks, food, and a flashlight may be all you need. Consider your own situation and take it from there)
- Laminated maps of area traveling (If leaving area and unfamiliar with where you are headed)
- GPS tracker
- Cellphone with recharger and/or extra battery
- A few days’ worth of medications and way to administer (insulin vial, syringe, etc.)
- Snack bars and boxed juices, bottled water
- Extra pair of socks, shoes, hats, and gloves
- Hand warmers
- Raincoat or poncho
- Headlamp and flashlights with batteries
- Basic first aid kit
- If traveling with child still in diapers make sure have extra, plus wipes
- Whistles with lanyard to signal for help
- Extra blankets, sleeping bags, etc.
- Tow strap
- LED road flares
- Shovel and small bag of kitty litter for under wheels stuck on ice
A few other considerations:
- Let someone know where you are going, route and when expected to arrive.
- Take into consideration passengers if traveling by car. Ages, needs, and if stranded for long period of time activities like color books, etc. for children.
- Remember to always try to keep your gas tank at least half full. Even short commutes can turn treacherous. Inclement weather can cause gas shortages.
- Top off windshield wiper fluid, use fluid rated for below freezing weather.
- Avoid rushing to the grocer during weather events by keeping pantry well stocked.
Over the past two years we have been subjected to upheaval on every level of our lives. What we thought was stable, consistent, and taken for granted is not the case.
Unlike regional disasters the global pandemic is and will continue to affect every facet of life. To put it bluntly, our infrastructure is crumbling before our very eyes.
Everyday life has been affected on every level. Chip shortages which are used in the manufacture of computers, appliances and our vehicles are headline news. The transportation industry has taken a hit. Ports are clogged with ships waiting to unload goods. Illness has prevented workers from working in the agricultural fields and meat processing plants. Avian influenza (bird flu) has affected flocks in several states. In Kentucky alone 240,00 chickens tested positive and will be culled.
The global pandemic has affected our way of life.
Our dependence on other countries for our medications is often overlooked.
All one has to do is to look at the list of medication shortages facing our country right now. As of this writing there are 165 listed.
Our dependence on China and India for medicines

In July 2019 the U.S.-China Economic and Security Review Commission held a hearing on the United States’ growing reliance on China’s pharmaceutical products. In the discussion, Gary Cohn, then chief economic advisor to President Trump, argued against a trade war with China by invoking a Department of Commerce study that found that 97 percent of all antibiotics in the United States came from China. “If you’re the Chinese and you want to really just destroy us, just stop sending us antibiotics,” he said.
According to Dr Sakthivel Selvaraj, Director, Health Economics, Financing and Policy, at the Public Health Foundation of India (PHFI) New Delhi, India imports almost 80% of active pharmaceutical ingredients (APIs) and intermediates from China, which is huge and needs be reduced. These ingredients are used in the manufacture of over the counter and prescription medications. India imports these ingredients due to the fact the production cost is 20-30% less in China.
Some of the medicines India relies on Chinas API to manufacture are:
- Paracetamol (Tylenol)
- Ciprofloxacin (Cipro)
- Metformin (Glucophage)
- Acetylsalicylic acid (Aspirin)
- Ofloxacin (Floxin)
- Metronidazole (Flagyl)
- Ampicillin (Antibiotic)
- Amoxicillin (Antibiotic)
- Ascorbic acid (A form of vitamin C)
- Intermediates, on the other hand, are chemical compounds that are used in producing APIs.
In March 2020 India banned 26 drugs from export. A month later they lifted the ban on 24 of these drugs due to pressure from the U.S. At any time, a country could shut its export doors, due to political pressure, illness, transportation logistics, shortage of APIs or other reasons.
Will there be more medication shortages?
Given the fact that our dependence on vital, lifesaving antibiotics and other drugs is in the hands of other countries, until we can start to source and produce these medications in our country the outlook is very poor.
On a positive note: In August of 2021 the FDA approved a, USAntibiotics , based out of Bristol, Tennessee to produce two of the most widely prescribed antibiotics , Amoxicillin and Amoxicillin Clavulanate.
In addition, in response to the Cares act the National Academy of Sciences, Engineering and Medicine will conduct a study to examine the security of the medical product supply chain and provide recommendations. This study and implementation will take time. Our infrastructure will need a major overhaul to implement this.
This is a step in the right direction, however
What can we do?
Action Plan
- Get out your notebook and go to your medicine cabinet. Pull out all your creams, drops, supplements and any other treatments you have. Write them down. Start with prescription medications first. Check the amount and refills you have left. If this is a medication for a chronic conditions (Diabetic, high blood pressure, etc.) Do you have enough to get you by for a few months if supply chain is disrupted or totally collapses? When is your next appointment to get these medications refilled? If you are running low contact your medical provider and ask for a few months stock to have on hand in case of supply disruption.
- How are your other medical supplies stocked? If you are low on antibiotic ointment, burn cream, bandages, get those stocked as well.
- Be prepared. A well-stocked medicine cabinet with emergency antibiotics is a step forward in the right direction. Antibiotics can treat many infections before they become life threatening: Strep throat, skin infections, travelers’ diarrhea, animal bites, urinary tract infections, ear infections to name a few.
Be prepared. The hard fact is that our supply chain is disrupted, and it isn’t coming back anytime soon.

 Add to this state and federal agencies warn healthcare providers of imminent cyberattacks.
Add to this state and federal agencies warn healthcare providers of imminent cyberattacks.